Introduction
There can be extreme joy with snow sports. Excitement. Adrenaline. The breathlessness experienced after achieving a perfect run or, through luck or skill, narrowly avoiding catastrophe.
That’s a good day.
A bad day?
When gravity, weather and snow conditions, fatigue or a momentary lack of concentration combine, you catch an edge, and host a yard sale*. Or worse still, you suffer an injury worthy of a Ski Patrol rescue that keeps you away from the snow for the rest of the season. Maybe permanently.
Of course, prevention is better than a cure so, do your best to prepare for your chosen activity on the slopes. Snowsafe Australia has some great advice for safety and preparation. https://www.snowsafe.org.au/alpine-safety but that’s a whole different subject.
This blog is about injuries common to snow sports and how to manage them.
The Numbers

According to the Australian Institute of Health and Welfare (AIHW) https://www.aihw.gov.au/reports/injury/sports-injury-hospitalisations-2019-20/contents/sports-participation-and-rates-of-injury, the reported number of injuries for snow sports against the number of participants for 2019 – 20 aged 15 and over, was 5 per 1000.
So how many people are skiing and snowboarding?
Approximately 277,000 participants in snowboarding and skiing for 2019 – 20 aged 15 and over, according to AusPlay. Add another thousand or five for children under 15 years!
Safety on the slopes
There is some great information on how to manage an accident while skiing or snowboarding on the Snowsafe website ( https://www.snowsafe.org.au/accident )
Here is a brief over of the main points you need to know in case of an accident on the slopes.

To get to the casualty you should approach from the side or up from below their position, especially if the slopes are icy.
If the slopes are icy it is important to keep your skis or snowboard on. If you can take them off, cross your skis, or place your board upright in the snow, uphill from the casualty. If possible you can also get someone to stand uphill of the casualty to give a warning to others using the slope.
Do not remove the casualty’s skis or snowboard, and leave the casualty where they are if it is safe to do so.
Reassure the casualty and keep them warm. Wait for the ski patrol.
Injuries
From the AIHW, in 2019-20 there was a total of 1,654 hospitalisations due to Winter sports injuries. 59% of those were injuries due to falls.
The most common injuries were fractures at 60% with dislocations and soft tissue injuries combined at 27%
Fractures mean broken bones: arms, legs, ribs. Dislocations and soft tissue injuries refer to dislocated joints: shoulder, knee, wrist, and soft tissue injuries: sprains and strains of wrists, ankles, muscles, and tendons.
Concussion from head injuries is always a concern.
It is recommended that the Ski Patrol manage all first aid on the slopes. However, there may be occasions when they are delayed, not available, or you are some distance away from them such as cross-country skiing.
If this is the case you may have to provide some First Aid to the casualty.
Joints
When muscles, tendons and ligaments are cold they have less elasticity and are therefore more prone to injury. It is also well known that sporting performance is reduced in cold conditions. When these two factors combine, falls are more likely and injuries are usually more severe.
Statistically, ligaments and muscles acting on the joints of the knees, shoulders, wrists, and spine are the most common soft tissue injuries from falls while skiing or snowboarding.
Joints absorb shocks and give us movement; ligaments support parts of the joints and tendons join the muscles to the bone.
As mentioned before, Joints connect bones. They provide stability to the skeleton and allow movement.
Joints are held together and supported by ligaments. Smooth cartilage prevents friction as the bones move against one another.
In freely movable joints, the entire joint is enclosed inside a membrane filled with lubricating synovial fluid, which helps to provide extra cushioning against impact.
In general, the greater the range of movement, the higher the risk of injury. This is because the strength of the joint is reduced.
There are different types of joints allowing different movements.
- Ball and socket joint – where the rounded head of one bone sits within the cup of another, for example, the hip joint or shoulder joint. Able to move in all directions
- Saddle joint – allows movement back and forth and from side to side, but does not allow rotation, such as the joint at the base of the thumb.
- Hinge joint –where the two bones open and close in one direction only such as the knee and elbow joints.
- Condyloid joint –movement without rotation, such as in the jaw or finger joints.
- Gliding joint –where the smooth surfaces slip over one another, allowing some movement, such as the wrist joints.
Common joint injuries include
- Dislocations – when two connected bones slip out of position in a joint.
- Fractures and breaks
- Sprains and strains – of the Ligaments and Tendons around the joint
- Overuse injuries such as tendonitis – making the same movements repeatedly over time, the body’s joints and surrounding tendons and muscles become irritated and inflamed.
- Osteoporosis – bones that are weakened from a loss of bone density, due to a lack of calcium. As a result, the bones that make up the joint may break easily.
Signs and Symptoms of a dislocation
- Pain, Swelling, and Bruising
- Instability of the joint and or Loss of ability to move the joint
- Visibly deformed joint where the bone looks out of place
Management of a dislocation
DO NOT try to replace or reduce a dislocation. Leave that for the Ski Patrol, Ambulance or Medical Professional.
Follow these steps:
- If the injury is to a limb: Check for any circulation and if absent, move the limb gently to try and restore it.
- Call 000 for an ambulance, or in this case, Ski Patrol.
- Place and support the limb using soft padding and bandages.
- Use icepacks, if possible, over the joint.
- If the shoulder is dislocated, support the arm in a position of least discomfort use a sling if needed and apply an ice compress.
- If the wrist is dislocated, support using a sling and apply an ice compress.
When using ice, make sure to apply it for ten minutes with 1 Hour rest in between or 20 minutes on / 2hrs off
Sprain and Strains
The difference between a sprain and a strain is that a sprain injures the bands of tissue that connect two bones together, while a strain involves an injury to a muscle or to the band of tissue that attaches a muscle to a bone.
Ligaments are bands of tough elastic tissue around your joints. They connect bone to bone, give your joints support, and limit their movement. You have ligaments around your knees, ankles, elbows, shoulders, and other joints.
A Sprain is when a ligament supporting a joint is overstretched or torn. Sprains commonly happen in the ankle, knee, or wrist.
Strain
Strains on the other hand occur when a tendon, or muscle, is overstretched or torn.
Tendons are tough, flexible, and inelastic bands of fibrous connective tissue that connect muscles to bones.
Strains are often the result of repetitive movements and from overtraining without adequate time for rest and muscle repair in between workout sessions.
Common areas affected by strains are the leg, foot, calf, groin, hamstring and back.
Signs and Symptoms for Strains and Sprains
This include:
- Pain, bruising and swelling in the affected area
- Sudden pain in the affected area along with loss of power in the affected limb
- The muscle in the affected limb is tender to the touch
Management
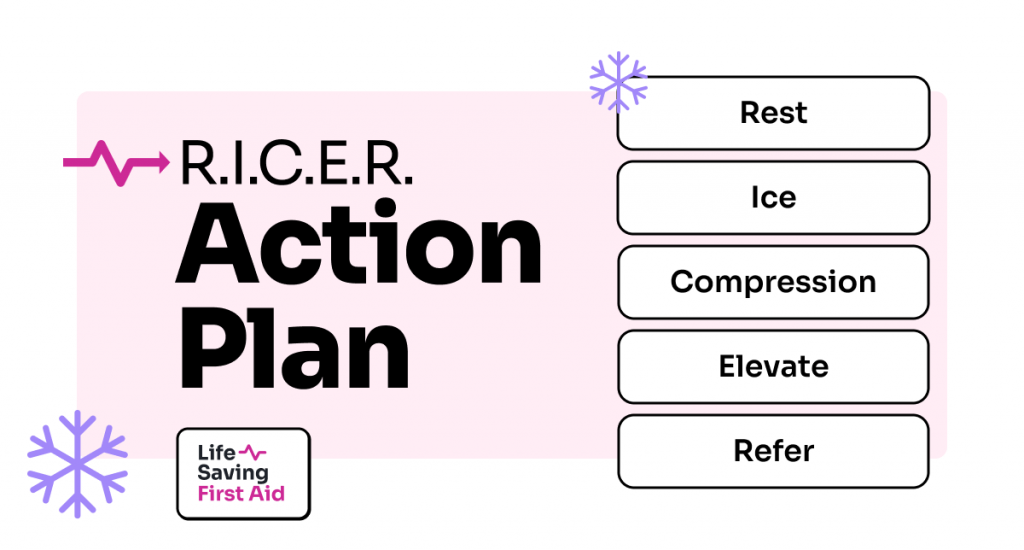
To manage strains and sprains we can follow our R.I.C.E.R. action plan
- Rest – encourage the casualty to stop any activity and make them comfortable
- Ice – Apply an icepack, wrapped in cloth, to the injured area
- Compression – apply an elastic bandage, if available, over the injured area. Not too tight, you need to allow for circulation
- Elevate – elevate the injured area above their heart height if practical
- Refer – refer them to a medical professional to have the area looked at.
When treating using R.I.C.E.R. you should also do no Harm.
NO
- Heat – apply no heat to the injury
- Alcohol – No alcohol
- Running – so no activity that might affect the injury
- Massage – do not massage the injury.
This method should be used within the first 48–72 hours (depending on severity) after the injury to speed up the recovery process.
Fractures
Fractures, although painful, are often not life-threatening injuries. However, it is important they are managed correctly to ensure the healing process – around four to eight weeks to heal, depending on the age and health of the person and the type of break – can run its course without any disruptions such as infection, permanent deformity, or lifelong disability.
There are different types of bone fractures. Some are more severe than others, depending on the strength and direction of the force, the bone involved, and the person’s age and general health.
As a First Aider, it is important you can recognise the different types of fractures so you can apply the correct First Aid.
Different types of fractures include
- Closed or simple fracture – the broken bone has not pierced the skin
- Open or compound fracture – the broken bone juts out through the skin, or a wound leads to the fracture site.
- Greenstick fracture – A greenstick fracture occurs when a bone bends and cracks, instead of breaking completely into separate pieces. The fracture looks like what happens when you try to break a small, “green” branch on a tree. This can occur in children because their bones are more flexible than an adult’s bones
- Hairline fracture – the most common form is a stress fracture, often occurring in the foot or lower leg because of repeated stress from activities such as jogging or running
- Complicated fracture – structures surrounding the fracture are injured. There may be damage to the veins, arteries or nerves, and there may also be an injury to the lining of the bone (the periosteum)
- Comminuted fracture – the bone is shattered into small pieces. This type of complicated fracture tends to heal more slowly
- Compression fracture – occurs when two bones are forced against each other. The bones of the spine, called vertebrae, can have this type of fracture. Older people, particularly those with osteoporosis, are at higher risk.
It’s good to remember that not all fractures are of a person’s arm or leg. Trauma to the head, chest, spine, or pelvis can fracture bones such as the skull and ribs. And, if this isn’t bad enough, these fractures are further complicated by damage to the underlying body parts that the bone normally protects for example the lungs or brain.
Some of these fractures can be difficult to manage using first aid only as they may be life-threatening injuries. Always call 000 ( Ski Patrol ) if you suspect this type of fracture.
Signs and Symptoms of bone fracture
The symptoms of a fracture depend on the particular bone and the severity of the injury but may include:
- Pain, swelling and bruising
- Deformity or an inability to use the limb
- A bone sticking out through the skin
- Grating noise when the limb is moved
Complications of a fracture may include
- Blood loss – bones have a rich blood supply. A bad break can make you lose a large amount of blood
- Injuries to organs, tissues, or surrounding structures – for example, the brain can be damaged by a skull fracture. Chest organs can be injured if a rib breaks
- Shock
Management
As with any First Aid incident, our primary action plan is DRSABCD and calling Ski Patrol or Triple Zero (000).
If you know the casualty has a broken bone, or you suspect a bone fracture you should
- Keep the person still – do not move them unless there is an immediate danger, especially if you suspect a fracture of the skull, spine, ribs, pelvis, or upper leg
- Attend to any bleeding wounds first. Stop the bleeding by pressing firmly on the site with a clean dressing.
- If a bone is protruding, apply pressure around the edges of the wound
- If bleeding is controlled, keep the wound covered with a clean dressing
- Never try to straighten broken bones
- For a limb fracture, provide support and comfort such as a pillow under the lower leg or forearm. However, do not cause further pain or unnecessary movement of the broken bone
- Use a sling to support an arm or collarbone fracture
- Raise the fractured area if possible and apply a cold pack to reduce swelling and pain. Do Not raise the fractured area if it causes the casualty further pain or discomfort
- Stop the person from eating or drinking anything until they are seen by a doctor, in case they need surgery
- Reassure and monitor their condition and if you feel you need medical help call triple zero (Ski Patrol) for an ambulance
Apply a splint to the fractured limb. Splints do not have to be professionally manufactured. Items like wooden boards and folded magazines can work for some fractures. You should immobilise the limb above and below the fracture using padding between the splint and the limb. If you can, apply two splints placing one on each side of the fracture.
It is also a good idea to use wide bandages if possible to check the casualty’s circulation in both the area of the injury and throughout their entire body.
For a fractured arm, support the limb with a sling.
Head Injuries – Concussion
A concussion is common in snowsports and can be challenging to identify and manage across sporting settings, from recreational environments to elite teams.
A concussion is a mild traumatic brain injury that follows some trauma to the head, is usually diagnosed by a doctor and symptoms of concussion can persist for up to three weeks after trauma.
Advise the casualty to be alert for any danger signs over the next one or two days, such as
- persistent vomiting,
- loss of coordination, or
- bad or worsening headaches despite pain-relieving medication
Any trauma to the head may result in a concussion. And sometimes the signs and symptoms of concussion are difficult to recognise.
It is especially important that all casualties who have sustained a head injury, regardless of severity, seek assessment by a health care professional or at a hospital.
Well, that was a fairly large blog, but it has given you some excellent information ( If I do say so myself…) And for those unaware of the meaning of “Host a yard sale” when used in snow sports. According to the Urban Dictionary – “When a skier or snowboarder eats it on the slopes and loses all of their gear.”
If a skier loses his skis, poles, hat, goggles, and anything else, you can shout “YARD SALE” from the ski lift above him.
For all you gapers and Jerrys out there https://hankinmtn.com/ski-and-snowboard-slang-dictionary/ and https://www.redenergy.com.au/living-energy/lifestyle/snow-culture-and-etiquette, you might learn something!
And lastly, for more on Head and spinal injuries, check out my blog on that subject. https://lifesavingfirstaid.com.au/blog/
Well, that’s that. Until next time….. Stay safe