Winter
We all know how cold, wet, and miserable this time of year can be in most parts of southern Australia.
However, winter is also the season when millions – 4,1882,000 in 2019 to be exact! – of people make their annual pilgrimage to the Victorian snowfields of the Australian Alps, and the phrase “Don’t go out there…. It’s FREEZING!”, becomes meaningless and is ignored.
Of those 4.1 million almost half are day visitors which means over 2 million will stay at least one night on whatever mountain they are visiting.
As with any concentration of people there is a risk of injuries. Combine that concentration with physical activities such as skiing, snowboarding, hiking etc, and you increase that risk of injury many times over.
In this post I am going to talk about Hypothermia and frostbite. The follow up post, Part 2 will cover physical injuries you may encounter on the snowfields, sprains and strains, broken bones, head injuries etc.
Body
Our bodies constantly adapt their temperature to environmental conditions. Our internal body temperature, our CORE temperature is regulated by a part of our brain called the hypothalamus.
The hypothalamus checks our current body temperature and compares it with the normal body temperature of about 37°C.
If our temperature is too low, the hypothalamus makes sure that the body generates and maintains heat. If, on the other hand, our current body temperature is too high, heat is given off or sweat is produced to cool the skin.
The hypothalamus automatically adjusts keep our internal body temperature at an average of 37°C.
If our core temperature falls below, 37°C then we may experience Hypothermia.
What is Hypothermia?
Exposure to cold conditions can lead to generalised cooling of the body, localised cold injury and or HYPOTHERMIA. (a combination of the prefix hypo-, meaning “below,” and the word thermē, which translates from the Greek as “heat.)
Hypothermia occurs when the body’s temperature drops below 35°C. and it cannot warm up by itself.
As the body temperature falls, systems and organs progressively fail until death occurs.
Hypothermia may develop rapidly, for example by falling into icy water.
However, it is more common that hypothermia is a gradual process, such as, when someone experiences prolonged exposure to cold conditions such as cold weather or lying on a cold floor or buried under snow by an avalanche.
Infants and the elderly are at a greater risk of hypothermia.
Infants because they have a larger surface area compared to body weight so they can lose body heat faster than older children and adults.
And the elderly, their ability to become aware of temperature change is impaired due to the loss of nerve endings to the skin. Less fat on their body which has an insulating function, and a lower metabolic rate, means they generate less body heat themselves.
Ok, how does the body lose heat anyway?
Well basically there are four ways that the human body loses heat:
conduction – by direct transfer from the body to an object that is cooler than the body (for example, lying on a cold surface will pass body warmth to the surface away from the body)
convection – air or liquid flow across the skin drawing off heat (for example, wind will increase heat loss, as will water that is cooler than body temperature)
radiation – electromagnetic waves distribute heat into the ambient environment (for example, exposed skin will allow heat to be drawn off if the air temperature is less than the body – the exposed head of a person is a strong source of heat loss, particularly in children)
and
evaporation – fluid on the skin turns to vapour, drawing off heat (moist skin will lose heat more rapidly, such as in someone who is wet, clammy or has exposed moist skin, such as burns).
So now you understand why it is so important to stay dry, sheltered from the wind, wearing good quality, warm clothing when enjoying our wonderful snow-covered peaks.
Oh… and don’t forget… keeping your feet warm and dry as well.
What happens when body temperature starts to fall?
A couple of things usually occur which can indicate that the person’s body temperature is falling and they, and their bodies, are trying to keep warm.
They are:
- Behavioural – the person will try and move around to generate heat and seek shelter from further heat loss. And
- Physiological – the body moves blood from the extremities to the core to keep it warm,
- body hair stands on end to trap a layer of warm air around us (goose bumps),
- we shiver to make more heat
and - our body (the hypothalamus) releases hormones to speed up our metabolism to create more heat.
If these measures don’t work, yep you guessed it, hypothermia will result.
Signs and Symptoms
So, as I mentioned earlier, hypothermia is usually a gradual process with the person going through various stages.
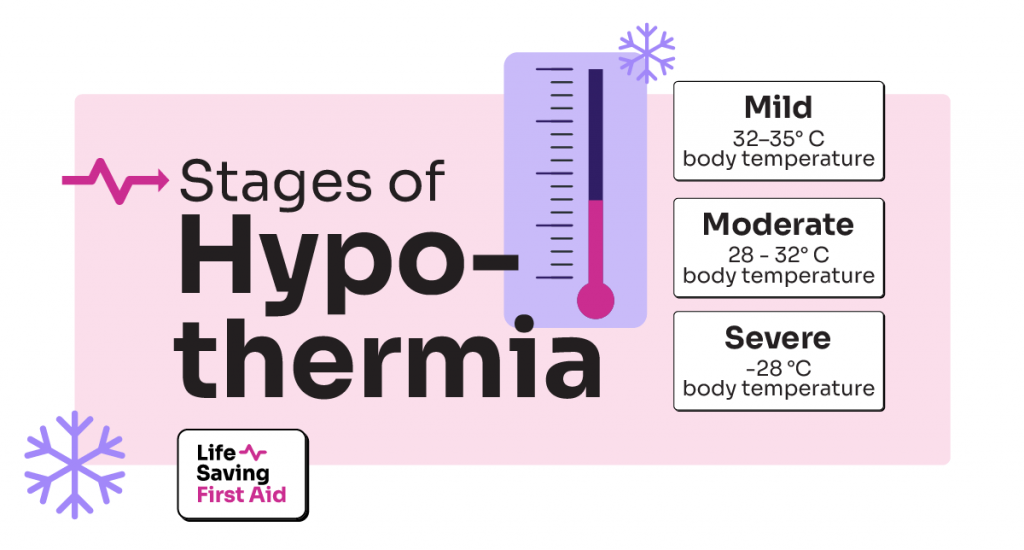
Mild hypothermia – 32–35 °C body temperature
- The casualty will be shivering – the body trying to keep warm by stimulating muscles
- their skin will be pale and cool – blood supply restricted to keep internal organs warm
- They may have impaired coordination, slurred speech with possibly delayed responses.
Moderate hypothermia – 28 – 32° C body temperature
- The casualty will stop shivering and experience increasing muscle stiffness.
- They will be confused and become less responsive.
- Their blood pressure will drop, and they will have a slow, irregular pulse
Severe hypothermia – Less than 28° C body temperature
The casualty may display all the signs and symptoms of moderate hypothermia as well as
- be very cold to touch, unresponsive, rigid,
- dangerous heart rhythms
- cardiac arrest
- Or they may appear lifeless with, fixed and dilated pupils, particularly if they have a weak slow pulse.
Never assume a person is dead. A person with severe hypothermia may only take one breath per minute, with a heart rate of less than 20 beats per minute. (2)
Management of Hypothermia
When you notice the signs of hypothermia, you should apply the following guidelines:
- Follow DRSABCD. Don’t forget you need to be aware of your own risk of developing hypothermia in cold environments and should monitor your own status as well as that of the affected person
- Dial Triple Zero (000) for an ambulance if the casualty’s condition is severe.
- If possible, move the casualty to a warm, dry place, remove any wet clothing from the casualty and if they are fully conscious give them a warm sugary drink, no alcohol or coffee.
- Avoid any excess activity and help the casualty to lay down in a comfortable position.
- Warm the casualty with blankets or an emergency blanket making sure you cover the casualty’s head to maintain body heat. You can also use body to body contact to warm the casualty
- Use heat packs and place them on the neck, armpits, or groin. Be careful not to burn the casualty.
- Reassure and stay with the casualty until medical aid arrives.
Freezing cold injury also known as Frostbite
Frostbite occurs when tissues freeze.
This happens in cold environments when blood vessels constrict and reduce blood flow and oxygen to the extremities such as the fingers and toes, however, it can affect any part of the body.
Management of a freezing cold injury is the same as for severe hypothermia plus rewarming of the affected parts.
- When rewarming, it is important that you warm them up slowly. Use body heat and blanket DO NOT rub the affected tissue or use radiant heat i.e., sit by a fire.
- Affected fingers may be placed in the opposite armpit, the armpit of a companion, or a warm hand over a frostbitten cheek or ear while feet can be reheated on the warm abdomen (under clothing) of a companion
- If you have rewarmed frostbitten body parts you must ensure that re-freezing does not occur.
Remember to continually monitor the casualty’s breathing–if their breathing stops, start cardiopulmonary resuscitation (CPR) immediately. Continue CPR until the person starts breathing on their own, medical help arrives, you become exhausted, or it becomes too dangerous to continue.
Once the colour and consistency of the skin have been restored, the person can safely resume normal activity, provided they increase their insulation and take precautions against recurrence i.e., refreezing.
One last note, if you are a fan of the “Apre Ski” activities all toasty by the chalet fire, with a snifter of brandy or whatever you prefer to warm your toes, be aware of the effect of alcohol on your body.
Alcohol relaxes the blood vessels allowing more blood to flow near the skin and this makes people feel cosy, giving a flushed appearance, and a warm sensation.
Blood flowing near the skin increases the rate of heat loss, and the alcohol slows down your metabolism, which slows down internal heat generation.
If you have had too much to drink, there is now a significant risk of hypothermia if you go outside in cold weather.
Alcohol also impairs judgement, so you are less likely to recognise the environment, your own physical condition, and then less likely to take protective measures against heat loss.
This also applies to any other mind-altering substance.
Just to recap the main points
- In all cases of hypothermia, the first thing to do is to prevent any further heat loss. Do this by removing the four ways that heat loss occurs mentioned earlier i.e.: conduction, convection, radiation, and evaporation.
- Follow DRSABCD. Don’t forget you need to be aware of your own risk of developing hypothermia in cold environments and should monitor your own status as well as that of the affected person
- If possible, move the casualty to a warm, dry place, remove any wet clothing from the casualty and if they are fully conscious give them a warm sugary drink, or coffee.
- Warm them slowly – body heat. No friction or radiant heat from the fire.
- no alcohol – Don’t be PISSED on the PISTE!
If you DO go to the snow even for just a day trip remember keep warm and dry and watch out for your family and friends.
Well, that’s that. Until next time….. Stay safe
Adrian