What is an Allergic Reaction?
Allergic reactions are a significant health concern that can impact individuals drastically, varying from mild discomfort to life-threatening emergencies. An allergic reaction occurs when the immune system responds abnormally to a usually harmless substance called an allergen. These allergens can include foods, pollen, pet dander, or certain medications.
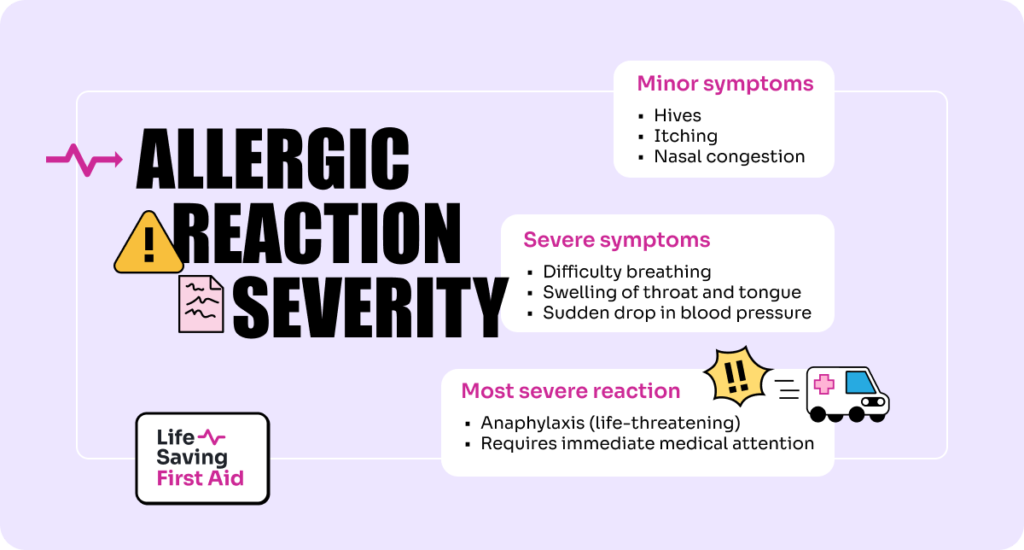
The severity of allergic reactions can range from minor symptoms like hives, itching, and nasal congestion to more severe symptoms such as difficulty breathing, swelling of the throat and tongue, and a sudden drop in blood pressure. The most severe form of allergic reaction is anaphylaxis, which can be life-threatening and requires immediate medical attention.
The impact of allergic reactions on an individual’s health and well-being can be profound. For those with severe allergies, daily activities can be overshadowed by the need to avoid triggers and the constant readiness to manage a possible emergency. This state of alert can induce anxiety and stress, affecting mental health and quality of life.
Understanding allergic reactions is crucial for effectively managing them, whether it involves avoiding known allergens, recognising the onset of a reaction, or knowing how to respond during an emergency. This awareness helps prevent severe health outcomes and supports a better quality of life for those affected
What Triggers an Allergic Reaction?
Allergic reactions are triggered when the immune system mistakenly identifies a typically harmless substance as a threat and mounts a defensive response. This overreaction by the immune system can be provoked by a variety of allergens, including foods, medications, insect stings, and environmental factors.
Common Allergens
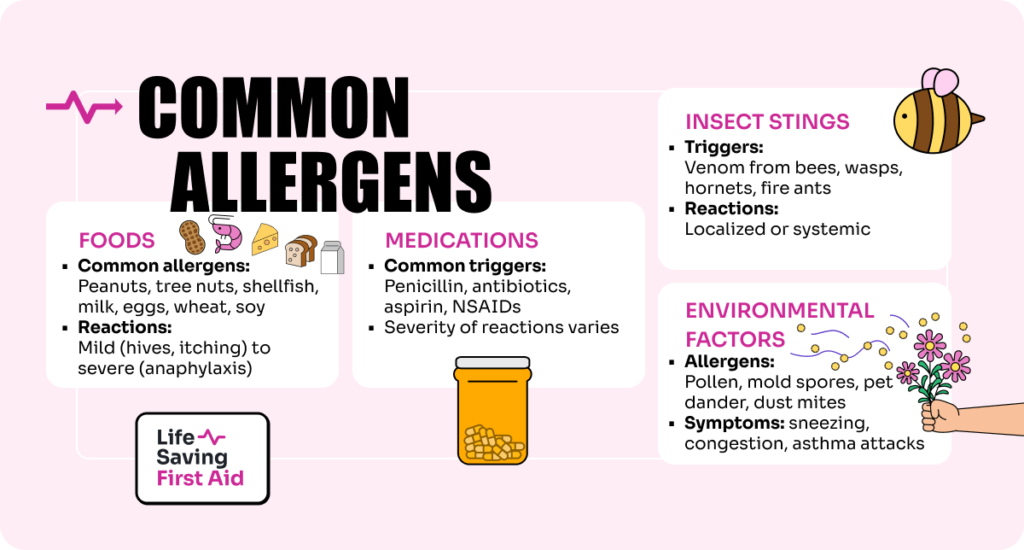
Foods: Some of the most common food allergens include peanuts, tree nuts, shellfish, milk, eggs, wheat, and soy. These foods can cause reactions ranging from mild symptoms, like hives and itching, to severe anaphylactic reactions.
According to the Centre for Food Allergy Research Australia – ” Australia is the allergy capital of the world with more than five million people living with allergies. Australia also has the highest rates of childhood food allergy globally, with one child in every classroom impacted. “
- Medications: Drugs like penicillin and other antibiotics, aspirin, and non-steroidal anti-inflammatory drugs (NSAIDs) are common triggers. Medication-induced allergic reactions can also vary widely in severity.
- Insect Stings: Venom from stings of bees, wasps, hornets, and fire ants are typical triggers. The reactions can be localised, affecting only the area around the sting, or systemic, affecting the whole body.
- Environmental Factors: Pollen from trees, grasses, and weeds; mould spores; pet dander; and dust mites are environmental allergens that often lead to respiratory symptoms, such as sneezing, congestion, and asthma attack.
Role of the Immune System
The immune system’s role in allergic reactions begins when it first encounters an allergen. In some individuals, the immune system views the allergen as a threat and produces Immunoglobulin E (IgE) antibodies. These antibodies attach to immune cells called mast cells and basophils that are found in various tissues throughout the body. When the individual is exposed to the allergen again, these antibodies recognise it and signal the immune cells to release histamine and other chemicals. This release causes the symptoms of an allergic reaction.
The intensity of the immune response can vary significantly among individuals and can even change over a person’s lifetime. Understanding the role of the immune system in these responses is crucial for developing effective treatments and preventive strategies, such as allergen avoidance, medications to control symptoms, and immunotherapy to reduce sensitivity to allergens.
Recognising and managing allergies effectively involves not only avoiding known allergens but also educating those affected about their condition and potential emergency responses, including the use of epinephrine auto-injectors in cases of severe reactions. This knowledge is vital for safeguarding health and improving the quality of life for individuals with allergies.
Symptoms of Allergies
Allergic reactions can manifest a wide array of symptoms, ranging from mild and merely inconvenient to severe and life-threatening. These symptoms can affect the skin, respiratory system, gastrointestinal tract, and cardiovascular system.
Mild to Moderate Symptoms
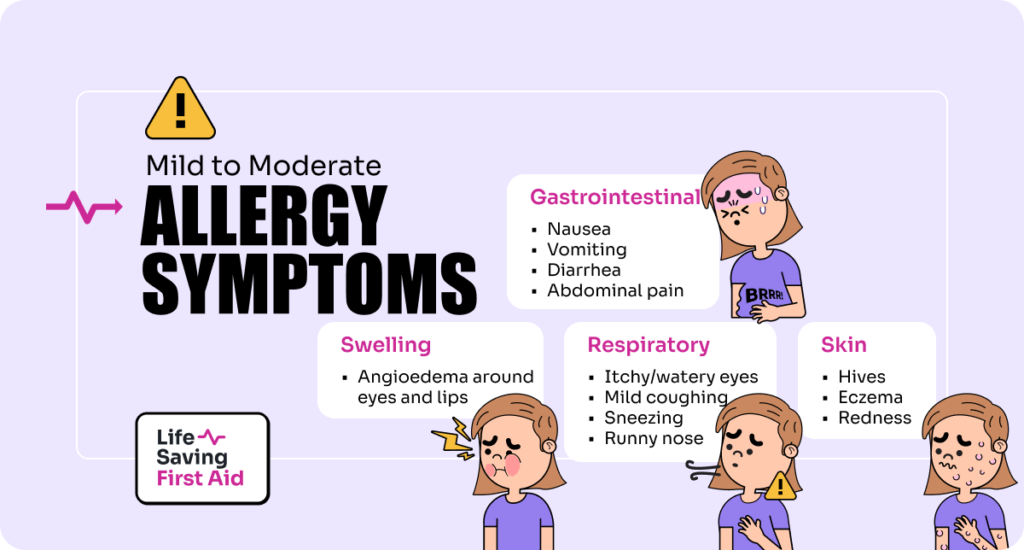
Skin Reactions:
- Hives: Raised, itchy, red welts on the skin’s surface.
- Eczema: A persistent rash that may produce scaly and itchy patches of skin.
- Redness: Skin can become red and irritated around the affected area.
Respiratory Symptoms:
- Sneezing and Runny Nose: Common in reactions to airborne allergens like pollen.
- Itchy and Watery Eyes: Often accompanied by redness and swelling of the eyelids.
- Mild Coughing: Triggered by irritation of the airways.
Gastrointestinal Symptoms:
- Nausea and Vomiting: The body’s way of expelling the allergen.
- Diarrhea: This can occur when allergens affect the gastrointestinal tract.
- Abdominal Pain: Cramping can occur due to inflammation in the gut.
Swelling:
- Angioedema: Swelling of the deeper layers of the skin, often seen around the eyes and lips.
Severe Symptoms
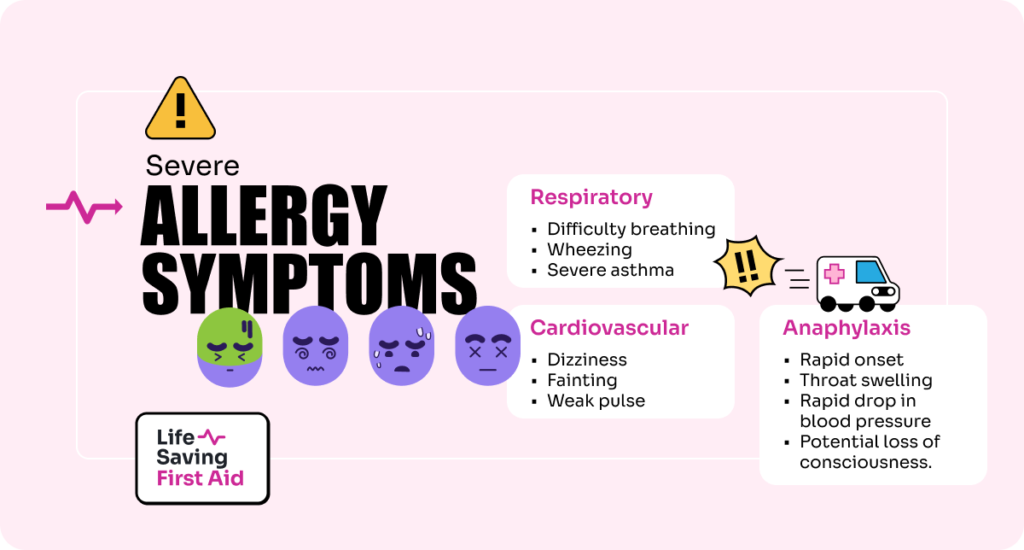
Respiratory Complications:
- Difficulty Breathing: Swelling in the throat or a severe asthma reaction can significantly restrict airways.
- Wheezing and Severe Asthma: Audible whistling sounds when breathing, indicative of obstructed airways.
Cardiovascular Symptoms:
- Dizziness or Fainting: Caused by a drop in blood pressure.
- Weak Pulse: A sign of anaphylaxis, indicating shock.
Anaphylaxis:
- A Severe, Whole-Body Reaction: This is a rapid onset emergency that can involve all the previously mentioned symptoms but with increased severity.
- Swelling of the Throat and Mouth: This can lead to difficulty swallowing and breathing.
- Rapid Drop in Blood Pressure: This can cause shock and organ failure if not treated promptly.
- Loss of Consciousness: Extreme cases can lead to unconsciousness within minutes.
What is Anaphylaxis?
Anaphylaxis is a systemic allergic reaction, which means it can affect multiple systems in the body simultaneously. It typically occurs within minutes of exposure to an allergen, but can sometimes take longer to manifest. Various allergens, including certain foods, medications, insect stings, or latex can trigger a reaction.
Symptoms of Anaphylaxis
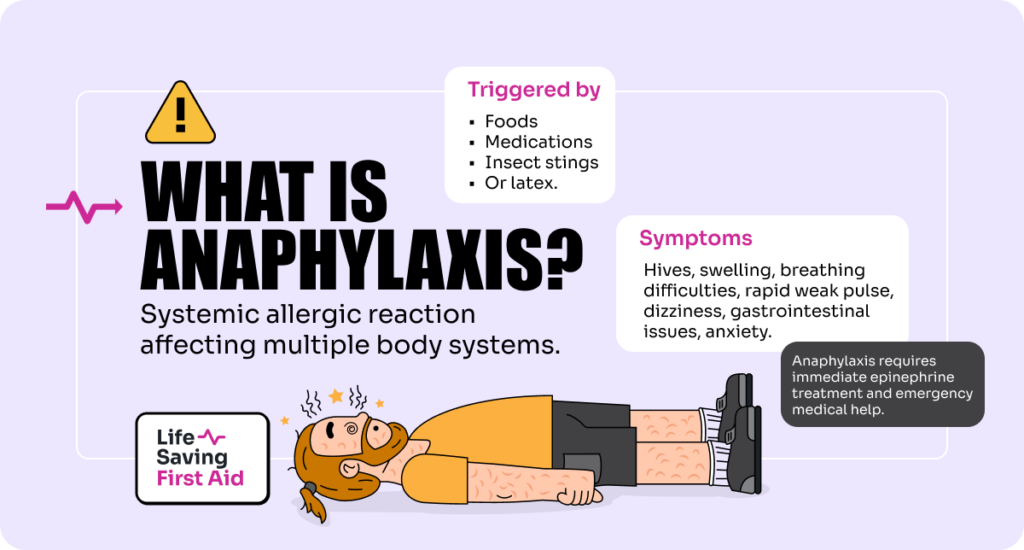
The symptoms of anaphylaxis can develop quickly and escalate from mild to severe. Key symptoms include:
- Skin reactions: such as hives, flushed skin, or pale skin
- Swelling: which can occur in the face, throat, lips, tongue, or other parts of the body
- Breathing difficulties: due to swelling in the airways or a severe asthma response
- Rapid, weak pulse
- Dizziness or fainting: as a result of a sudden drop in blood pressure
- Gastrointestinal symptoms: such as nausea, vomiting, diarrhea, and abdominal pain
- The feeling of impending doom: anxiety, or confusion
Anaphylaxis can quickly progress to cause breathing difficulties and vascular collapse, leading to shock and potentially, if untreated, death. Immediate treatment with epinephrine, commonly administered through an auto-injector like an EpiPen, is crucial. Epinephrine works by reversing the symptoms of anaphylaxis: it increases blood pressure, reduces swelling, and opens the airways. After administering epinephrine, it’s vital to call emergency services and seek professional medical help, as further treatment may be necessary, and symptoms can recur.
Creating an Anaphylaxis Action Plan
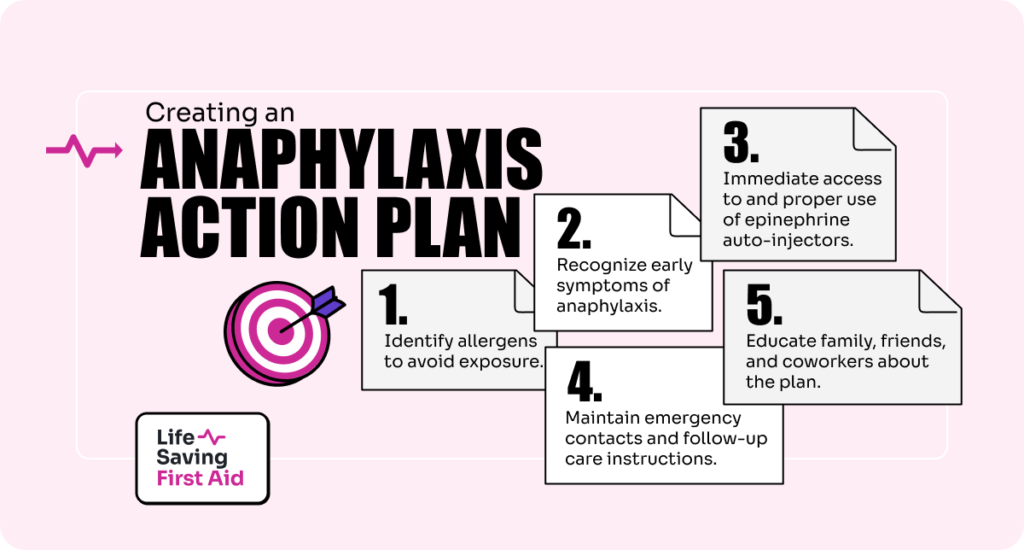
Having an anaphylaxis action plan is essential for anyone at risk of such reactions. An effective plan typically includes:
- Identification of Allergens: Knowing what triggers your allergic reactions is crucial to avoid exposure.
- Symptom Recognition: Understanding the early signs of anaphylaxis can help in taking swift action.
- Immediate Use of Epinephrine: Keeping an epinephrine auto-injector accessible at all times and knowing how to use it properly.
- Emergency Contacts: Having a list of emergency contacts and instructions for bystanders or caregivers on what to do and whom to call.
- Follow-Up Care: Instructions for seeking immediate medical care even after the symptoms subside, as secondary reactions can occur.
Educating family, friends, and coworkers about the action plan and how to use an epinephrine auto-injector can also be life-saving. Schools and workplaces should be aware of individuals with severe allergies to facilitate quick and effective responses in case of an emergency.
By preparing and adhering to an anaphylaxis action plan, individuals at risk can significantly improve their safety and outcomes in the event of an allergic emergency. This proactive approach not only saves lives but also provides peace of mind for those with severe allergies and their loved ones
Common Allergens
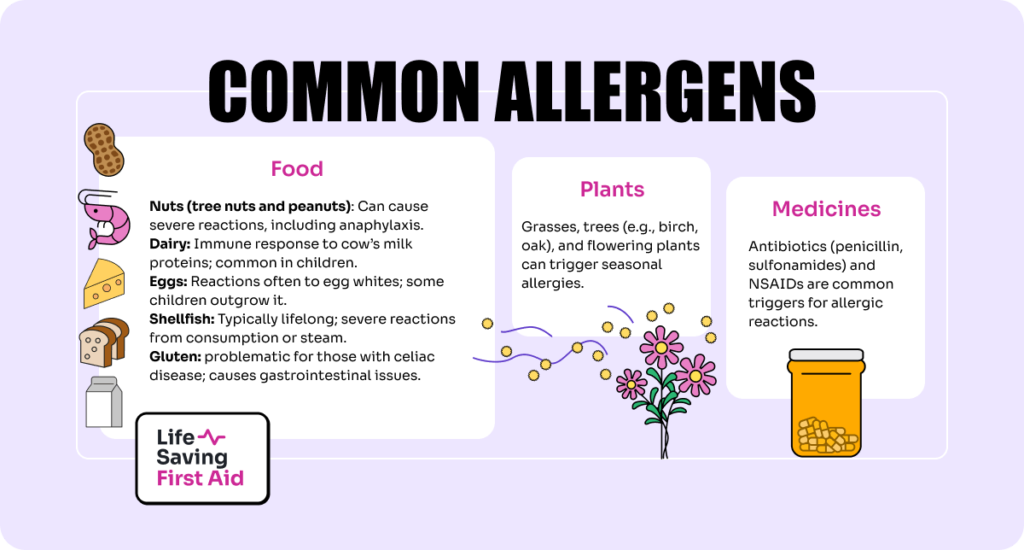
Allergic reactions can be triggered by a wide range of substances, known as allergens. The body’s immune system mistakenly identifies these typically harmless substances as threats, leading to an allergic response. Here’s an overview of the most common triggers of allergic reactions:
Food
1. Nuts
Nuts are one of the leading causes of food allergic reactions and can be divided into two categories: tree nuts and peanuts. Peanuts are legumes, similar to beans and lentils, but they are commonly grouped with nuts due to similar protein structures and allergic reactions.
- Tree Nuts: This category includes almonds, walnuts, hazelnuts, cashews, pistachios, and Brazil nuts. Reactions can range from mild to potentially life-threatening, including anaphylaxis.
- Peanuts: Despite being legumes, peanut allergies are often severe and can lead to anaphylactic reactions. Even trace amounts can trigger a response in highly sensitive individuals.
2. Dairy
Dairy allergies involve an immune response to one or more of the proteins present in cow’s milk, such as casein and whey. Symptoms can include hives, stomach upset, vomiting, and in severe cases, anaphylaxis. Dairy is a common allergen for children, although many outgrow it as they get older.
3. Eggs
Egg allergy is another common allergy, particularly among children. It typically involves reactions to proteins in the whites, but some people must avoid all parts of the egg. Symptoms range from skin reactions to respiratory issues and gastrointestinal discomfort. Like dairy, some children outgrow egg allergies.
4. Shellfish
Shellfish allergy is typically lifelong and can be caused by various types of shellfish, including shrimp, crab, lobster, and mollusks like clams, mussels, and oysters. The allergic reaction to shellfish can be severe, often occurring from both consuming shellfish or inhaling steam from cooking shellfish.
5. Gluten
Gluten is a protein found in wheat, barley, and rye. It is problematic primarily for individuals with celiac disease, a severe autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Symptoms include bloating, diarrhea, and abdominal pain, and can lead to serious complications if not managed with a strict gluten-free diet. A related condition, non-celiac gluten sensitivity, causes similar symptoms but without the intestinal damage.
Plants
Allergenic plants, particularly those that produce pollen, are major triggers for seasonal allergies, commonly known as hay fever or allergic rhinitis. These plants release tiny grains of pollen that are carried by the wind, often over long distances. When inhaled by someone who is allergic, these pollen grains can cause symptoms like sneezing, itchy and watery eyes, and a runny nose. Here’s a look at some common allergenic plants, categorised by grasses, trees, and flowers:
1. Grasses
Grass pollen is one of the most common allergens. The following grasses are known for producing significant amounts of pollen that can trigger allergic reactions:
- Bermuda Grass: Common in warmer climates, Bermuda grass releases pollen from late spring to fall.
- Rye Grass: Often used in lawns and fields, rye grass is a significant pollen producer in the spring and summer.
- Bahia Grass: Common in subtropical regions, its pollen is highly allergenic.
2. Trees
Tree pollen is typically released early in the year and can be highly allergenic. Some trees known for their high pollen output include:
- Birch: One of the most common allergenic trees, particularly in northern climates. Birch pollen is released in spring and can cause severe reactions in sensitive individuals.
- Oak: Pollenates in the spring and is known for its high allergenicity, which can severely affect those with allergies.
- Pine: Although less allergenic than others, pine trees produce large amounts of pollen that can still cause symptoms.
3. Flowers
While many people associate flowers with strong scents that can cause allergies, it’s actually the pollen from certain flowering plants that is more likely to be problematic for allergy sufferers:
- Daisy Family: Includes many flowering plants like chrysanthemums and sunflowers that can cause allergic reactions due to their pollen.
- Chrysanthemums: These flowers can trigger reactions due to their pollen and the presence of other plant compounds.
- Sunflowers: While beautiful, sunflowers produce pollen that can be allergenic to some people.
Medicines
Certain medications can trigger allergic reactions in some individuals, with antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) being among the most common culprits.
Antibiotics
Antibiotics are designed to fight infections by killing bacteria or preventing their growth. However, they can also be a common trigger for drug allergies. The mechanisms and manifestations can vary:
- Penicillin and Related Antibiotics: These are the most common antibiotics causing allergic reactions. The immune system can mistakenly recognise penicillin or its byproducts as harmful, leading to an immune response. Symptoms of an allergic reaction to penicillin may include rashes, hives, swelling, and in severe cases, anaphylaxis.
- Sulfonamides (Sulfa Drugs): While less common today, sulfa antibiotics can also cause severe allergic reactions. These may manifest as skin reactions, fever, and systemic symptoms.
- Cephalosporins: Similar to penicillin in structure, cephalosporins can cause cross-reactivity in individuals allergic to penicillin. Allergic reactions can range from mild to severe.
Non-steroidal anti-inflammatory Drugs (NSAIDs)
NSAIDs are commonly used to reduce pain, inflammation, and fever. They work by inhibiting enzymes involved in the production of inflammatory compounds. However, they can also trigger allergic reactions or exacerbate underlying conditions:
- Aspirin and Ibuprofen: These are among the most commonly used NSAIDs and can trigger allergies or other adverse reactions like asthma exacerbation. This is not always a true allergy but can be due to altered arachidonic acid metabolism, leading to an imbalance in prostaglandins and leukotrienes, inflammatory mediators that can cause respiratory symptoms in susceptible individuals.
- COX-2 Inhibitors: While designed to be safer for the stomach and less likely to cause gastrointestinal problems, COX-2 inhibitors can still trigger allergic reactions in some people.
Insects
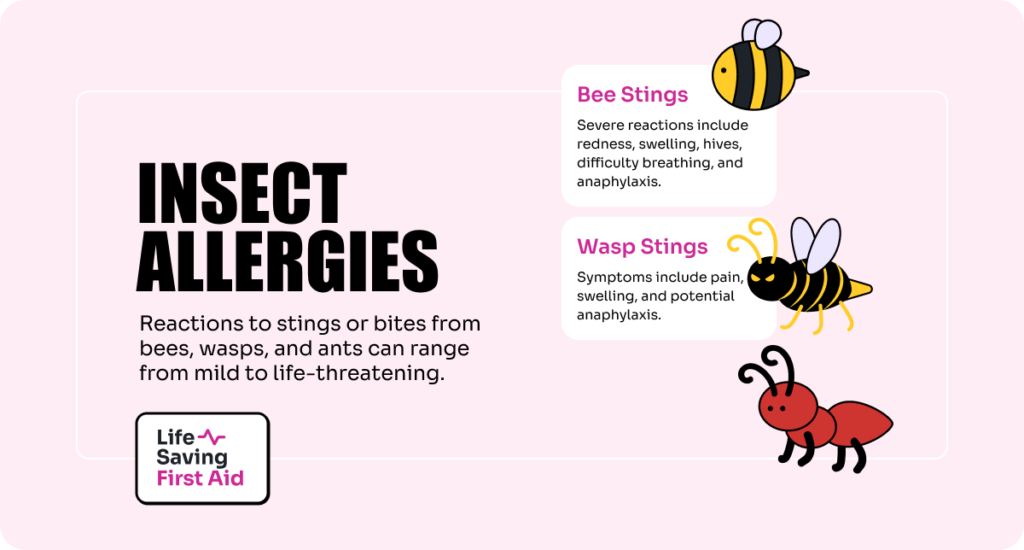
Allergic reactions caused by insect stings or bites, particularly from bees, wasps, and ants, can range from mild to severe and potentially life-threatening. These reactions are triggered when an insect injects venom into the skin during a sting.
1. Bee Stings
Bee stings are one of the more common causes of allergic reactions to insect venom. The venom contains proteins that affect skin cells and the immune system, causing pain and swelling at the sting site. In those allergic to bee venom, the reaction can be more severe, including symptoms such as:
- Extreme redness and swelling that increase for two or three days after the sting.
- Hives or rash that appears away from the sting site.
- Difficulty breathing due to swelling in the throat or lungs.
- Anaphylaxis that may include rapid swelling, difficulty breathing, a sharp drop in blood pressure, dizziness, or loss of consciousness.
2. Wasp Stings
Wasps can be more aggressive than bees and can sting multiple times, injecting venom with each sting. Wasp venom can cause significant allergic reactions similar to bee stings. Symptoms of a wasp sting reaction include:
- Pain, redness, and swelling at the sting site.
- Large areas of swelling may develop around the sting.
- Anaphylactic reactions in highly sensitive individuals, requiring immediate medical attention.
3. Ant Stings and Bites
Certain species of ants, like fire ants, not only bite but also sting by injecting venom. Fire ant stings can cause a unique reaction that includes:
- A sharp pain at the time of the sting followed by a red welt.
- The development of a blister filled with fluid on top of the welt within 24 hours.
- Multiple stings that often occur as fire ants latch on with their mandibles and inject venom multiple times in a circular pattern.
- In allergic individuals, symptoms can escalate to severe swelling, dizziness, breathing difficulties, or anaphylaxis.
Moulds
Allergic Reactions to Mould Spores
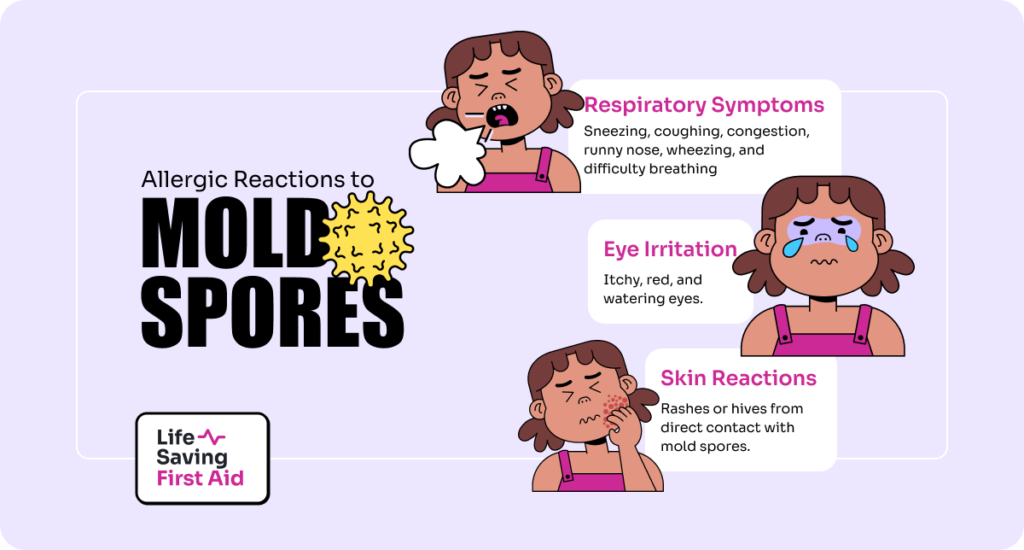
Mould spores can cause a variety of symptoms similar to other airborne allergens, such as pollen. Common allergic reactions include:
- Respiratory Symptoms: Sneezing, coughing, congestion, and runny nose are typical responses. People with mould allergies may also experience wheezing or difficulty breathing, especially if they have asthma.
- Eye Irritation: Itchy, red, and watering eyes are common in people exposed to mould spores.
- Skin Reactions: Some individuals might develop a rash or hives when exposed to mould, especially if they have direct contact with the spores.
Impact on Individuals with Asthma
For those with asthma, exposure to mould spores can be particularly problematic:
- Asthma Exacerbations: Mould spores can trigger severe asthma attacks, where symptoms such as wheezing, chest tightness, and shortness of breath become significantly worse.
- Increased Sensitivity: Continuous exposure to mould can increase sensitivity to mould spores, leading to more frequent and severe asthma symptoms.
- Long-term Lung Irritation: Prolonged exposure can cause persistent inflammation in the airways. This may lead to a decline in lung function over time.
Animal Dander
Pet dander from animals like cats and dogs is a common trigger for allergic reactions in many individuals. Dander consists of tiny, even microscopic, flecks of skin shed by cats, dogs, rodents, birds, and other animals with fur or feathers. These particles can carry proteins that are allergens. Allergens can cause allergic reactions when they come into contact with a person’s skin or are inhaled.
When people with allergies to pet dander inhale these particles or they come into contact with their skin, their immune system mistakenly identifies the proteins in the dander as harmful. This immune response can lead to various allergic symptoms such as respiratory symptoms, eye irritation, and skin reactions.
Pet dander is particularly troublesome because it is very small and lightweight, allowing it to remain airborne for long periods. It can also cling to clothing, furniture, carpets, and other surfaces in the home, making it difficult to completely eliminate.
Chemicals
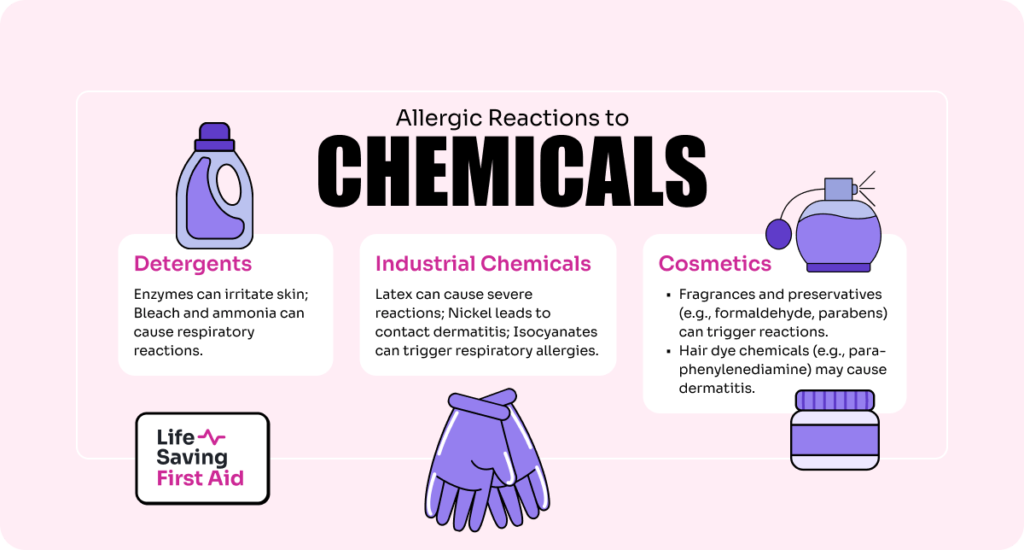
Allergic reactions to chemicals found in everyday products such as cosmetics, detergents, and industrial chemicals are a significant concern for many people. These reactions are often due to substances known as contact allergens, which can cause the immune system to overreact upon skin contact or inhalation.
Cosmetics:
- Fragrances and Preservatives: Many skin care products, perfumes, and makeup items contain fragrances and preservatives that can trigger allergic reactions. Common culprits include formaldehyde, parabens, and methylisothiazolinone.
- Hair Dye Chemicals: Para-phenylenediamine (PPD) found in hair dyes is a frequent cause of allergic reactions, leading to dermatitis on the scalp, face, or neck.
Detergents and Cleaning Agents:
- Enzymes: Laundry and dishwashing detergents often contain enzymes to break down stains and residue, which can cause skin irritation and allergic reactions.
- Bleach and Ammonia: These strong chemicals can cause respiratory and skin reactions in sensitive individuals.
Industrial Chemicals:
- Latex: Used in various products, including gloves and medical devices, latex can cause severe allergic reactions.
- Nickel: Found in everything from jewelry to coins and metal tools, nickel is a common cause of contact dermatitis.
- Isocyanates: Commonly used in paints, varnishes, and foam insulation, these chemicals can cause respiratory allergies and asthma.
Immediate First Aid for Allergic Reactions

Responding promptly and effectively to an allergic reaction can save lives, especially in cases of severe reactions like anaphylaxis. Here’s a step-by-step guide on how to respond to an allergic reaction, emphasising the importance of early symptom identification and the appropriate use of an EpiPen:
Step 1: Recognise the Symptoms
Identify signs and symptoms of an allergic reaction, which can include:
- Mild Symptoms: Hives, mild itching, nasal congestion, or minor swelling.
- Severe Symptoms (Anaphylaxis): Difficulty breathing, swelling of the throat or tongue, severe and rapid swelling, dizziness, fainting, abdominal pain, vomiting, or diarrhea.
Step 2: Evaluate the Severity
Quickly determine the severity of the symptoms. If any signs of severe allergic reactions (anaphylaxis) are present, proceed immediately to the next steps. For mild symptoms, monitor closely, as reactions can escalate quickly.
Step 3: Administer an EpiPen (for Severe Reactions)
If the individual has a history of severe allergies and carries an epinephrine auto-injector (EpiPen):
- 1 – Hold the EpiPen with the orange tip pointing downward.
- 2 – Remove the blue safety cap.
- 3 – Place the orange tip against the middle of the outer thigh.
- 4 – Push down firmly until a click is heard, then hold for 3 seconds.
- 5 – Remove the injector.
Step 4: Call Emergency Services
Call emergency services immediately if you observe severe symptoms, even if epinephrine has been administered.
Inform them that someone is experiencing a severe allergic reaction and mention if you have administered epinephrine. Be prepared to provide details about the person’s exposure.
Step 5: Follow Up with Care
If epinephrine was used, the individual must go to the hospital or a medical facility for further observation and care:
- After-effects: Biphasic anaphylaxis is when the reaction could recur.
- Monitoring: Medical professionals will monitor vital signs, administer additional medications if needed, and provide further treatment.
Step 6: Observe and Comfort
While waiting for emergency services:
- Keep the person lying flat, elevate their legs to improve blood flow, and cover them with a blanket.
- Do not give them anything to drink.
- If breathing becomes difficult, loosen tight clothing and ensure nothing is obstructing their airways.
- Stay with the person until medical help arrives.
Step 7: Prevention and Planning
After an allergic reaction:
- Review and revise: Consider what triggered the reaction and how exposure can be avoided in the future.
- Medical review: Schedule a follow-up with an allergist to potentially update treatment plans and discuss preventive strategies.
- Educate and inform: Ensure that family, friends, and co-workers are aware of the allergy, recognise the signs of an allergic reaction, and understand how to use an EpiPen.
Be Prepared: Learn How to Handle Allergic Reactions
In this blog, we’ve explored the critical aspects of allergic reactions, from recognising the variety of triggers including foods, insects, chemicals, and environmental factors to understanding the range of symptoms that can arise. We discussed the severity of reactions, particularly anaphylaxis, and the importance of being able to quickly identify and respond to such emergencies.
Key Takeaways:
- Understanding Allergens: Knowledge of common allergens, such as specific foods, pollen, pet dander, and medications, is crucial for prevention and preparedness. Avoiding known triggers is the first step in managing allergic reactions.
- Recognising Symptoms: Being able to identify the early signs of an allergic reaction, from mild symptoms like hives and itching to severe symptoms like difficulty breathing and swelling, can be lifesaving. This awareness is essential for timely and effective intervention.
- Emergency Response: Knowing how to respond to an allergic reaction, particularly anaphylaxis, is vital. This includes the proper administration of an EpiPen and immediately calling for medical help. Remember, epinephrine is the first line of defense in treating severe reactions and can prevent more severe consequences if administered quickly.
- Preparedness and Education: Having an allergy action plan and ensuring that those around you (family, friends, colleagues) are aware of it can make a significant difference in emergencies. Education about allergies and emergency responses should be ongoing.
- Medical Follow-Up: After an allergic reaction it’s important to seek further medical evaluation and care. Especially if an EpiPen was used. This helps to ensure that the allergic individual is stable and provides an opportunity to review and adjust allergy management strategies.
Understanding allergic reactions and being prepared to respond are not just about personal safety. They are about community awareness and readiness. Whether you or someone you know has allergies, the knowledge and steps discussed here empower you to act confidently and promptly, potentially saving lives. Encouraging a wider understanding and readiness to act in allergic emergencies is an essential part of fostering a safer environment for everyone.
Check out some of our other Blogs here.
This is me, Mitch. Watch this space!