Introduction:
Australia is home to around 139 species of venomous snakes. This includes 109 land-based and 30 marine-based species. Not all of these are dangerously venomous. Approximately one-third of them are however so, you can see how important snake antivenom is.
How is snake antivenom made? It’s a pretty interesting story and process.
Snake Venom:
First, a bit about venom.
Snake venom is created in the modified salivary glands of the snake. It is a complex mixture of enzymes and proteins of various sizes, amines, lipids, nucleosides, and carbohydrates.
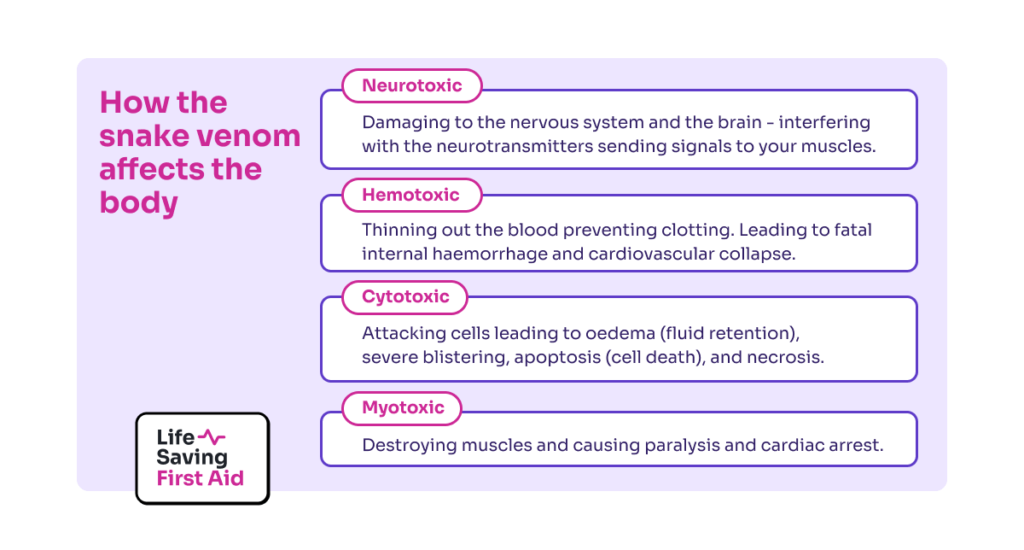
Snake venom affects the body in 4 different ways:
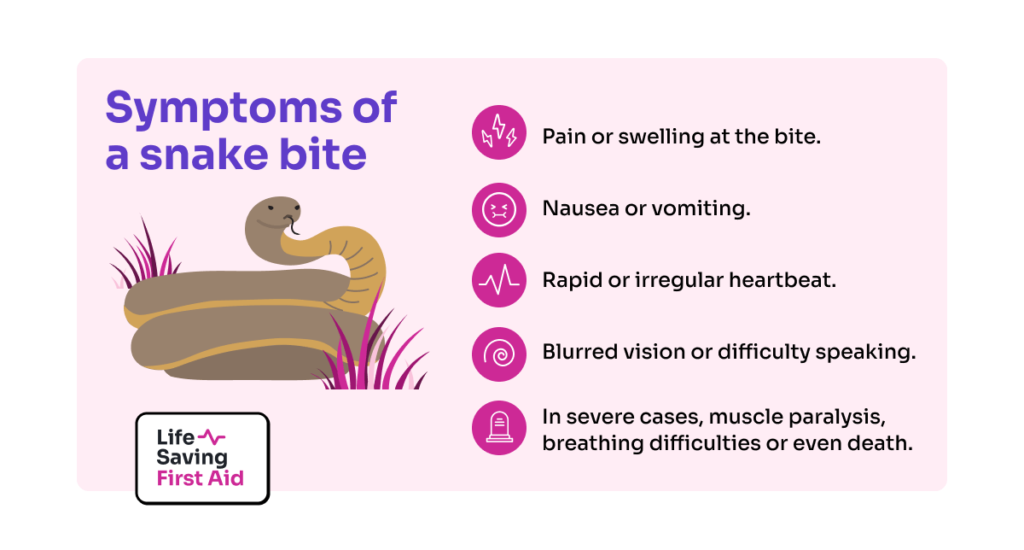
· Neurotoxic – Damaging to the nervous system and the brain – interfering with the neurotransmitters sending signals to your muscles.
· Hemotoxic – Thinning out the blood preventing clotting. Leading to fatal internal haemorrhage and cardiovascular collapse.
· Cytotoxic – Attacking cells leading to oedema (fluid retention), severe blistering, apoptosis (cell death), and necrosis.
· Myotoxic – destroying muscles and causing paralysis and cardiac arrest.
Some snake venom contains a mixture of all four types of toxins. Nasty Stuff.
Snakebite:
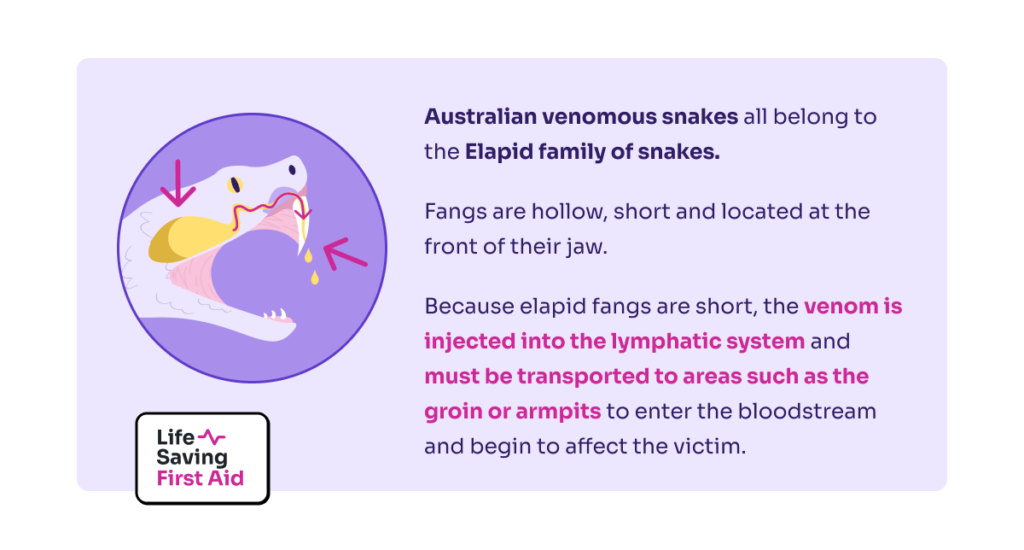
Australian venomous snakes all belong to the Elapid family of snakes and as such their fangs are hollow, short and located at the front of their jaw.
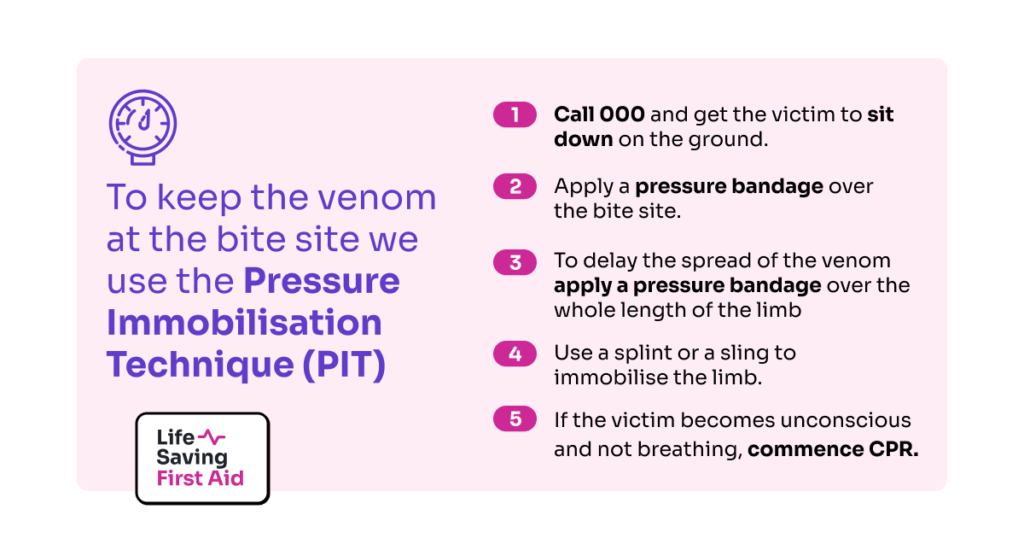
When the snake bites, venom is injected into the lymphatic system of the casualty. This happens because elapid snake fangs are short.
To enter the bloodstream and begin to affect the victim, the venom must be transported to areas such as the groin or armpits
The venom of the Elapidae family is primarily neurotoxic with some myotoxic effects.
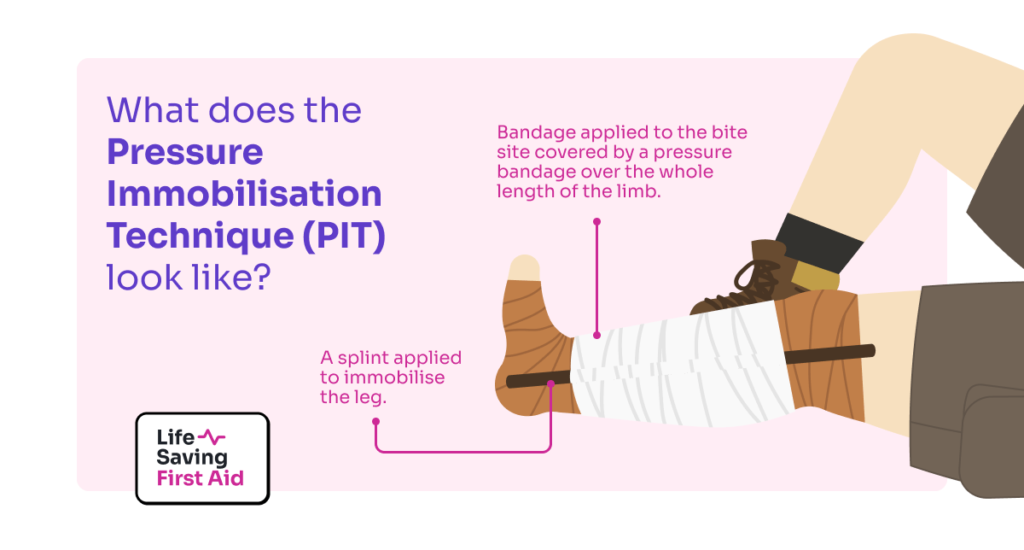
If you are treating a snake bite in Australia use the Pressure Immobilisation Technique – PIT. Click HERE for details of this technique.
Antivenom – A Brief History:
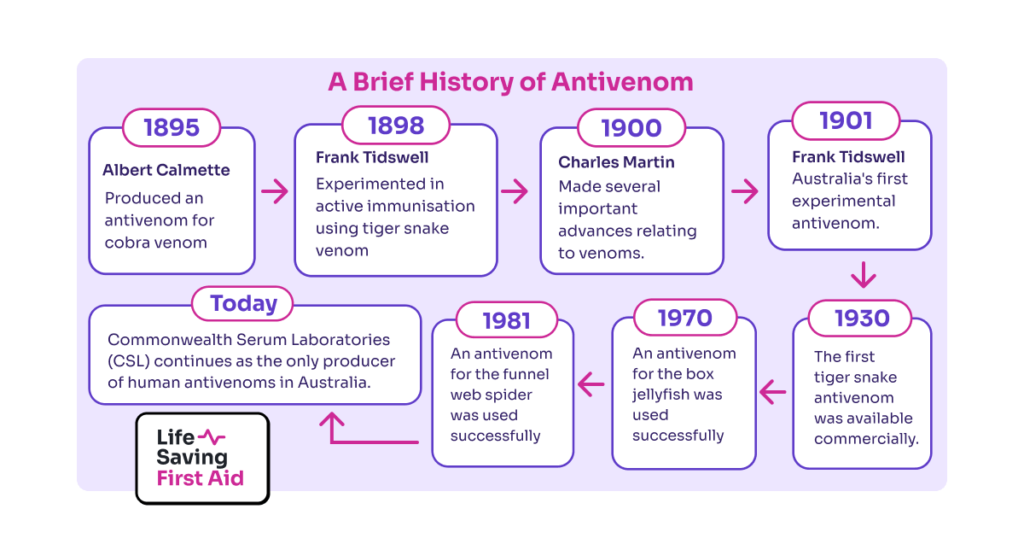
Albert Calmette, a French physician produced an antivenom for cobra venom in 1895 which was to revolutionise the treatment of snakebite worldwide.
In 1898 here in Australia, Frank Tidswell undertook pioneering experiments in active immunisation using tiger snake venom. Then in 1901, he produced Australia’s first experimental antivenom.
Around 1900 Charles Martin (Universities of Sydney and Melbourne) made several important advances relating to venoms. Including:
· Proving that Calmette’s anti-venom did not work for every snake.
· Conducting the first investigations into the chemistry of Australian venoms.
· Observing the action of venom on the body and its systems.
· Proposing that intravenous injection could be used to administer antivenom
· Concluding that the dose of venom injected influences the volume of antivenom used in treatment.
In 1928, research was led by Frank Morgan from Commonwealth Serum Laboratories (CSL )and Neil Fairley and Charles Kellaway from the Walter and Eliza Hall Institute (WEHI) into antivenom for Tiger snake and by October 1930 the first tiger snake antivenom was available commercially.
“While CSL had produced experimental antivenoms for many species it wasn’t until July 1955 that Australia’s second commercial snake antivenom for the taipan was released. This was followed by antivenoms for the brown snake (1956), redback spider (1956), death adder (1958), black snake (1959), stonefish (1959) and sea snake (1961). In 1962 a polyvalent snake antivenom was released to treat victims where the snake was unknown.
In 1970, an antivenom for the box jellyfish was used successfully. One for the funnel web spider followed in 1981. Today CSL continues as the only producer of human antivenoms in Australia”.(Source: Venoms & Antivenoms at Museum Victoria)
As you can see, Australia played an important role in antivenom research.
Hmm. That’s great…But get to the point! How we make snake antivenom?
Antivenom production:
Antivenom works by stimulating the production of antibodies. The immune system produces antibodies to neutralise dangerous antigens like viruses and bacteria. Antigens can also be effective in neutralising venom.
Antivenom does not destroy the venom’s toxins or reverse the venom’s effects on the body. However, the antibodies the antivenom creates can suppress the venom’s toxins preventing their spread and making them harmless.
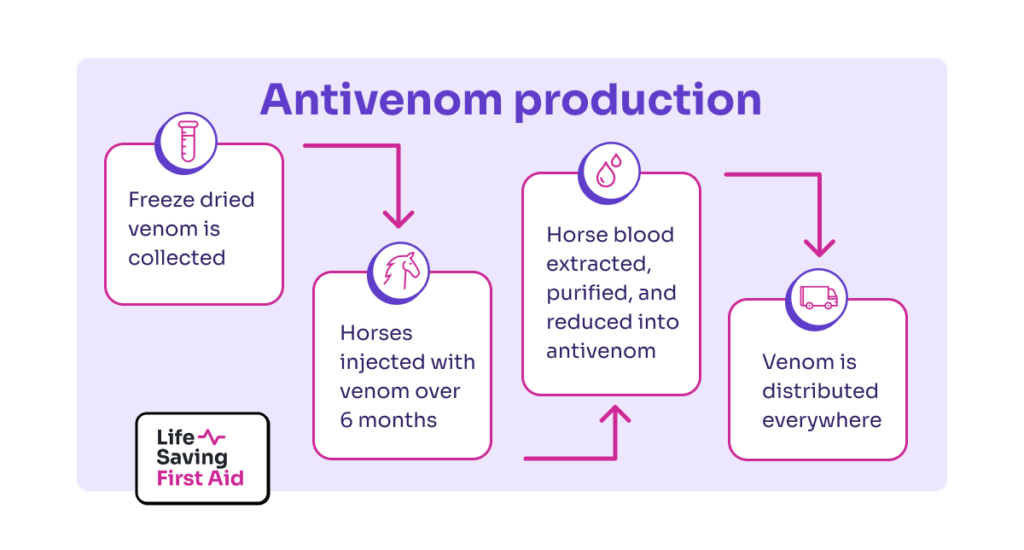
To make antivenom you need venom. Lots of it. The Australian Reptile Park, located in the central coast region of NSW has been the sole supplier of terrestrial snake venom for the purpose of making antivenom.
At the Australian Reptile Park, snake handlers milk 250 venomous snakes every fortnight. The Collected venom is freeze dried and the crystals are packaged and sent to be made into antivenom.
Australia uses horses for the production of all snake antivenom. Over a period of six months, the horses are injected with increasing doses of venom. During this time, they build up antibodies to the snake venom.
Blood is taken from the horses and the antibodies in the blood are extracted. These are purified and reduced to a usable form ie Antivenom.
( Oh, and by the way..the horses have a great life and suffer no inconvenience from this process. )
Then the antivenom is distributed (read SOLD..) to whoever needs it.
Which Antivenom for which snake?:
Identification of the snake will assist with the choice of the right antivenom for that snake. It will also indicate to the doctor the particular features and characteristics of envenomation by that type of snake.
Identification of snakes by the casualty, general public or by hospital staff is often inaccurate.
Sometimes, the snake is not even seen or is only glimpsed getting away. In these cases, a snakebite venom detection kit may be used.
Australia is the only country in the world that has snake venom detection kits.
The kits consist of a fast-acting two-step enzyme immune test in which wells are coated with antibodies to the various snake venoms.
The doctor will take a swab from the bite site and use the antibodies to determine the type of snake antivenom to be used.
Other Anti-Venoms:
As you are aware, Australia is home to lots of other venomous creatures. Fortunately, we have anti-venom most of the dangerous ones.
- Funnel-web spider – produced in Rabbits
- Redback Spider – produced in Horses
- Aust. paralysis Tick – produced in Dogs
- Box Jellyfish – produced in Sheep
- Stonefish – produced in Horses

Conclusion:
Thanks to the early research, Australia is in a fortunate position. We have good antivenom. Combined with good ambulance service and a good hospital system they all work together to reduce the impact of venomous bites on our community.
You should, of course, carry a snake bite kit with you…Just in case.
Last word from WC Fields:
“Always carry a flagon of whiskey in case of snakebite and furthermore always carry a small snake.”
Well, that’s that. Until next time…Stay safe.