Introduction
Australia is crawling with insects of one kind or another. In this article, we will look at first aid for bites and stings from various insects and spiders.
Recognising the Signs, Symptoms and knowing first aid management of insect bites and stings is important.
According to the Australian Institute of Health and Welfare, over 3,500 Australians were hospitalised due to contact with a venomous animal or plants in 2017–18. More than a 26% of these hospitalisations were caused by bee stings, almost 19% were caused by spider bites with redbacks the most common spider involved.
In Australia deaths from venomous plants, animals or insects is rare. The National Coronial Information System records 19 deaths in 2017–18 due to contact with venomous animals – 7 with venomous snakes, 12 with bees and wasps.
Bees, Wasp and Ant bites and stings
Lets’ have a look at bee, wasp and ant stings. Single stings from a bee, wasp or ant, can be painful but rarely cause serious problems except for persons who have a severe allergy to the venom.
However, multiple insect stings can cause severe pain and widespread skin reaction. Multiple stings around the face can cause severe local swelling and difficulty breathing even if the person is not allergic to that insect.
Bees
Here in Australia, there are over 1,500 native bee species in a range of shapes and sizes. Bees are critical to the sustainability of our food supply. An astonishing one-third of Australian food is dependent on honey bee pollination.
Australian native bees can be either solitary or social bees. On the other hand, honey bees will live together in a nest or hive. Honey bees are generally stronger pollinators, but the smaller native bees can access smaller flowers and also play an important role in pollination.
It is important to remember that bee stings leave behind the venom sac and sting which continues to inject venom into the skin, whilst a wasp or ant may sting multiple times without leaving a venom sac attached.
To remove the bee sting scrape sting out of the skin. Do no try to pull it out as you may squeeze more venom into the casualty.
Wasps
Wasps in Australia include European Wasps, English wasps and paper wasps all of which can sting and inject venom. Unlike a bee, the wasp does not lose its sting and therefore can sting you many times.
Stings from wasps can be immediately extremely painful with some redness around the bite area.
There can also be airway obstruction from swelling of the face and tongue due to anaphylaxis, or from many stings in or around the mouth.
Bull Ants
Bull ants are large, alert ants that can grow up to 40 mm They have characteristic large eyes and long, slender mandibles and a potent venom-loaded sting.
There are about 90 species of bull ants in Australia. Jumper ants are some of the smaller species. They have a habit of aggressively jumping toward intruders.
Ants deliver painful stings by gripping the intruder with their mandibles (jaws), curling their abdomen to reveal the sting, and injecting the victim with venom. Often the ant can deliver multiple stings.
Signs and Symptoms
Stings from bees, wasps and ants all show similar signs and symptoms
Minor reactions are usually immediate and intense local pain with some local redness and swelling.
On the other hand, more severe reactions can be airway obstruction from swelling of the face and tongue due to anaphylaxis, or from bee stings in or around the mouth. This may occur immediately or over several hours.
Management:
THE major immediate risk to the health of persons bitten or stung by insects is severe allergic reaction, Anaphylaxis.
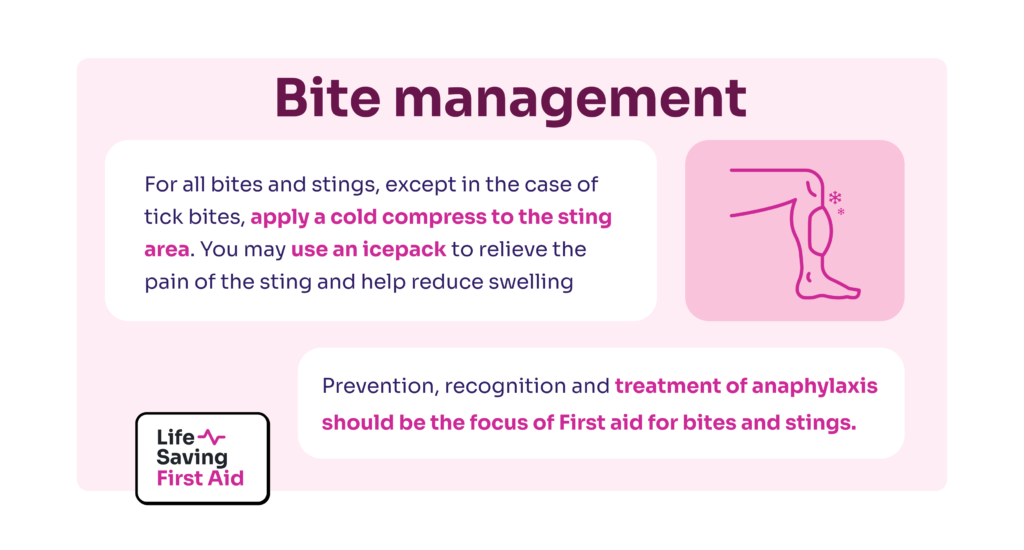
Prevention, recognition and treatment of anaphylaxis should be the focus of First aid for bites and stings.
For all bites and stings, except in the case of tick bites, apply a cold compress to the sting area. You may be use an icepack to relieve the pain of the sting and help reduce swelling
CALL 000 if multiple stings to the face or tongue have occurred or there is evidence of a severe allergic reaction anaphylaxis.
For anaphylaxis use an Epipen or other adrenaline injector to administer adrenaline (epinephrine) via intramuscular injection preferably into lateral thigh which is the outside part of the upper leg.
Monitor the casualty for any signs of allergic or other reaction
Ticks
Most tick bites cause few or no symptoms. Sometimes ticks may cause local skin irritation or a mild allergic reaction by injecting a toxin.
In susceptible people, a tick bite may cause a severe allergic reaction or anaphylaxis, which can be life threatening.
It may also occur in people with no previous exposure or known susceptibility.
To prevent it from injecting more allergen-containing saliva, do not forcibly remove or touch the tick
This will prevent allergic reactions due to allergen-containing saliva injected by the tick.
The safest way to remove a tick is to Freeze the tick, using a product that rapidly freezes and kills the tick, and allows it to drop off.
Alternatively, leave it in place and seek medical assistance to remove the tick as soon as possible.
If you must remove the tick, use fine tweezers, and grasp the head of the tick as close to the persons skin as possible and lever the tick out by the head. Do not squeeze the tick.
Monitor the casualty for any signs of allergic or other reaction.
Conclusion
The main points for first aid for bites and stings are:
• There are many insects in Australia that can bite and sting but generally they cause only minor problems
• Be aware of possible severe allergic reactions and manage accordingly
• Remove bee stings by scraping them out as soon as possible
• Apply cold pack to insect bite site for pain management – except for ticks
• Remove ticks, if possible, by freezing or tweezers applied to the tick’s head. Seek medical attention if you cannot remove the tick.
Well, that’s that. Until next time… Stay safe.