Introduction
I want to talk about the CPR discrepancy and closing the gap, one rescue at a time.
Do you know that females in cardiac arrest are less likely to receive out-of-hospital cardiopulmonary compressions (CPR) than males? That is simply because the provision of bystander CPR is less likely to be performed on a female by a member of the public. This is the CPR discrepancy.
Cardiac arrest:
A cardiac arrest is a life-threatening emergency situation where these casualties require immediate chest compressions to imitate the pumping of the heart, which promotes blood and oxygen delivery to the brain and other vital organs.
Despite the severity and complexity surrounding a cardiac arrest, the initial life-saving treatment simply involves using two hands to administer chest compressions in the centre of the chest, hard and fast.
However, despite the simplicity of performing CPR, recent literature states that only 39% of women received CPR from bystanders in public compared to 45% of males. (American Heart Association)

CPR on Women:
So, let’s unpack why the provision of CPR is less likely for Women and why the CPR discrepancy exists:
Gaining an insight into understanding the public perceptions of why the provision of CPR is less likely in women is an essential measure towards promoting the equitable implementation of CPR.
Bystanders are less likely to perform CPR on women due to concerns about inappropriate touching, potential accusations of sexual assault, or fear of causing injury.
Although these concerns for privacy and cultural sensitivity are valid, exposing the casualties’ chest must be done to initiate life-saving medical treatment. Using an Automatic External Defibrillator (AED) for example.
Exposing their chest includes removing all upper body clothing, which also includes removing or cutting their bras. This is optimal as it will allow for correct hand placement for compressions and for the AED electrode pads to be properly placed in the correct position. Further, as many bras include metal components, removing them reduces the risk of burns or electrical arcing during defibrillation.
Remember, exposing the female’s chest is necessary for optimal medical care. In the case of a woman with larger breasts, it might be required to lift the left breast with the back of your hand for accurate positioning of the AED pad. When a bra is removed and a female is lying on their back, it’s likely the breasts will fall to the side and thus allow for correct hand placement in the centre of their chest without the requirement to touch them. This is the correct location to effectively deliver compressions.
Preserving privacy:
Preserving the privacy of female patients can be achieved by continuing to treat them with dignity and respect at all times. It is important to ensure only those assisting with resuscitation are within sight of their exposed chest and for all other bystanders to maintain at a distance. In addition, capturing photos or videos of the casualty is inappropriate and unnecessary. Additionally, if there is a cloth or towel available, it can be used to cover the chest and preserve modesty, whilst compressions are provided.
CPR on pregnant women:
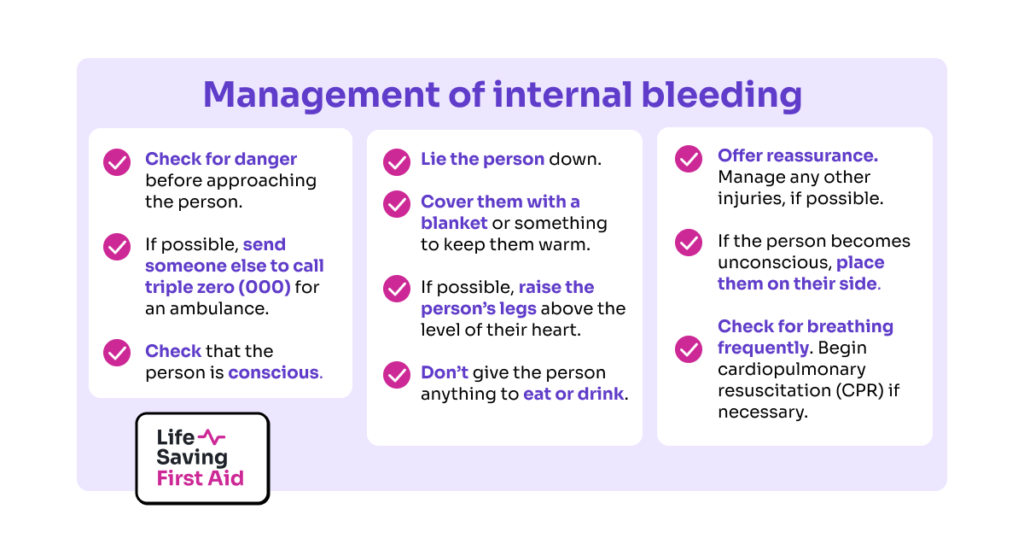
It is often misperceived that pregnant women who experience a cardiac arrest should not receive resuscitation with CPR and defibrillation. However, the standard protocol for resuscitation remains unchanged and it’s expected that they receive the same quality CPR and AED shocks as anyone else. Therefore, observing the same three life-saving procedures; calling 000, starting CPR, and utilising an AED as soon as possible is vital to attempt resuscitation.
Both compressions and defibrillation should not pose any significant risk to the mother or baby. However, there are some alterations we can practice to further mitigate any risks.
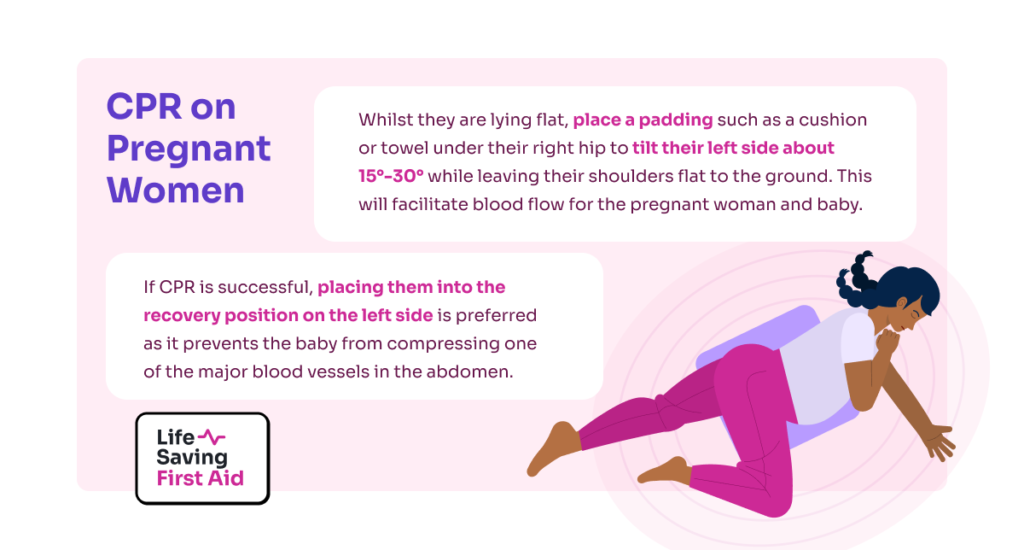
Whilst they are lying flat, place a padding such as a cushion or towel under their right hip to tilt their left side about 15°-30° while leaving their shoulders flat to the ground. This will facilitate blood flow for the pregnant woman and baby.
Finally, as for all patients, if CPR is successful, placing them in the recovery position whilst you wait for the ambulance to arrive is ideal. However, the left side is preferred as it prevents the baby from compressing one of the major blood vessels in the abdomen.
Conclusion:
Remember, if you attempt to resuscitate and save the life of a female casualty with genuine and well-intentioned efforts, you will always be protected under the Good Samaritan Legislation.
I hope this blog encourages strong public education and eliminates the biases surrounding bystander CPR on female casualties so we can make a difference together and save lives, regardless of gender, one rescue at a time.
Thanks for tuning in, see you in the next blog! – Dounia