Automatic External Defibrillator
AEDs. And how to use them. Here’s the shocking truth! An Automatic External Defibrillator (AED) is a life-saving device that can treat abnormal heart rhythms due to Sudden Cardiac Arrest (SCA), a condition where the heart unexpectedly stops pumping.
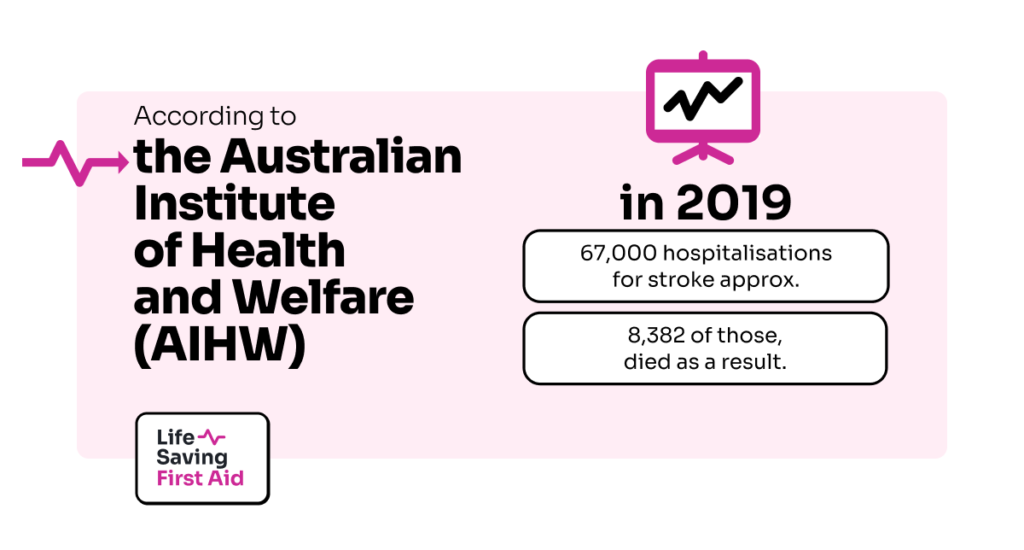
“Over 33,000 people experience an out-of-hospital cardiac arrest in Australia every year. Less than 9% will survive. The first 5 minutes after a person has a cardiac arrest are the most critical. For every minute that passes, the chance of survival decreases. Defibrillators can be used for certain cardiac arrhythmias which occur in around 20-30 per cent of all cardiac arrests. Early cardiopulmonary resuscitation (CPR) and defibrillation within the first 8-10 minutes can increase the chance of survival by up to 75 per cent.”
It’s important to know what defibrillators, or AEDs, are, how to find them, and how to use them.

What do they do?
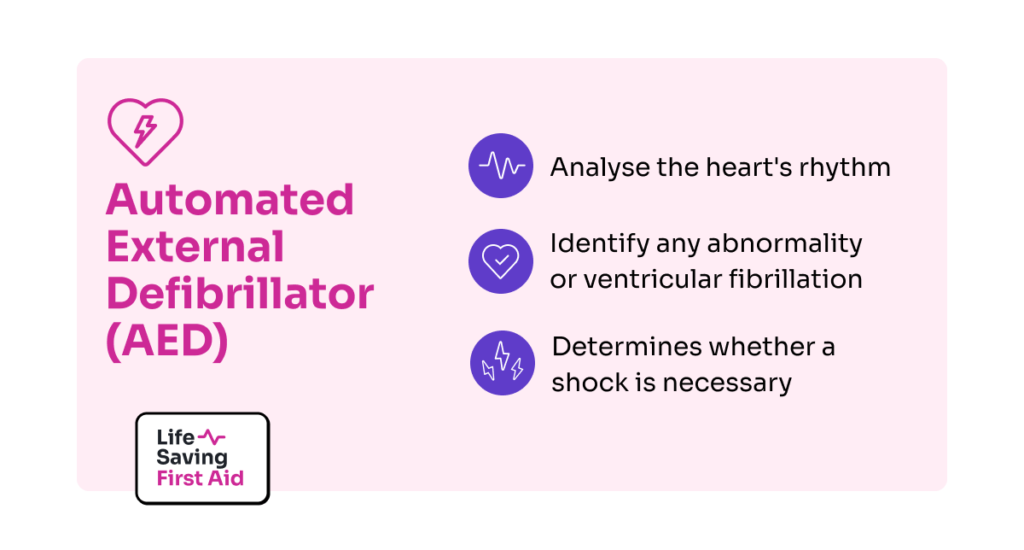
Defibrillation is the essential process of restoring the heart’s normal rhythm and is most effective within the first five minutes of a Sudden Cardiac Arrest. An Automated External Defibrillator (AED) can analyse the heart’s rhythm and identify any abnormality or ventricular fibrillation. The AED then determines whether a shock is necessary and delivers it if needed.
An AED will not restart a heart once it has completely stopped. As shown above, a defib will detect irregular heart rhythms and hopefully, shock them back to normal rhythms.
It is not designed to shock a heart back to life if it has stopped. Nor will it deliver a shock to a heart when it detects a normal heart rhythm.
That answers the question, “AEDs what are they”?
For – How to use them? Read on..
How to use.
Defibrillators are easy to use and provide voice prompts to guide users step-by-step. It’s best to start CPR while someone else retrieves the defibrillator.
They are designed for everyone to use and provide easy-to-follow voice prompts for guidance. While training beforehand is helpful, anyone can use a Defibrillator in an emergency.
However, completing First Aid training and refreshers can save precious time and increase confidence.
Early CPR increases the chance of keeping the heart in a shockable rhythm, improving the chances of survival.
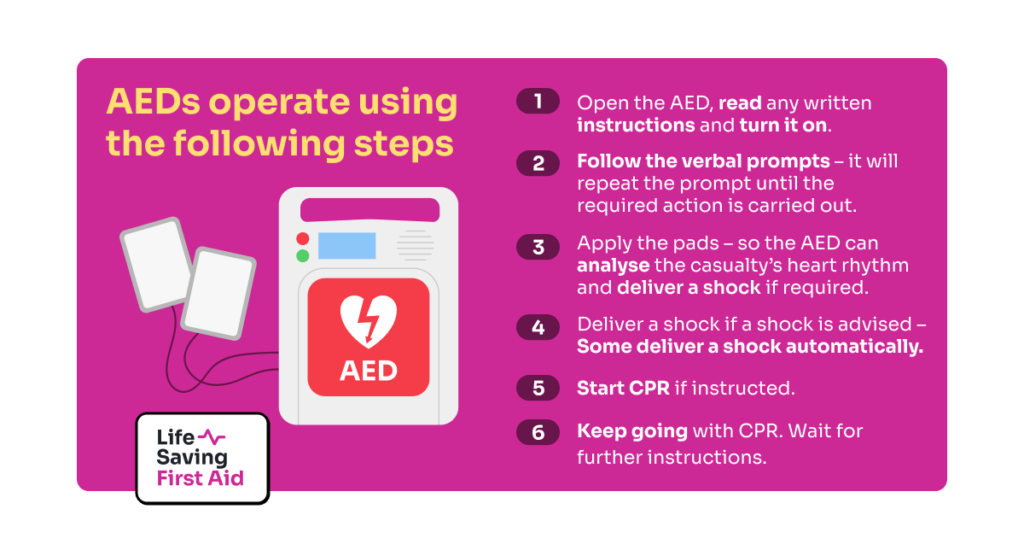
All AEDs basically operate using the following steps:
- Open the AED and turn it on. Some of them will start automatically upon opening.
- Follow the verbal prompts – it will repeat the prompt until the required action is carried out.
- Apply the pads – so the AED can analyse the casualty’s heart rhythm and deliver a shock if required.
- Deliver a shock if a shock is advised – Some deliver a shock automatically.
- Start CPR if instructed.
- Keep going with CPR. Wait for further instructions.
Remember to listen to, and follow, the instructions from the AED. Advise any bystanders to “Stand Clear”! when instructed to by the AED.
Simple!
Where can I find one?
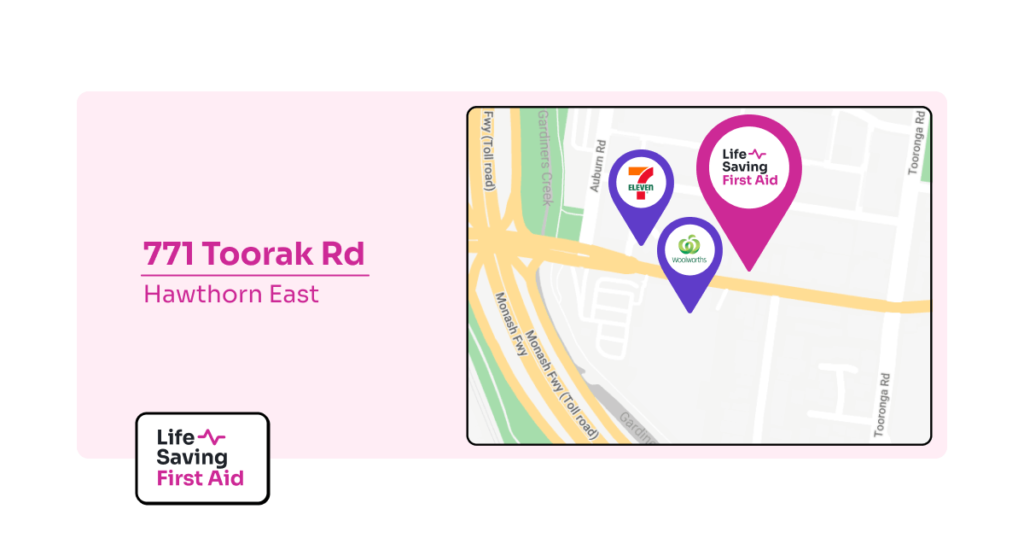
So, you have a good idea of how to operate a Defib… Now, you are probably thinking, “where can I get a defib if I am out and about”?
Well, you will often find one in your nearest:
- Hospital, Medical Centre
- School
- Community Centre
- Sporting clubs, shopping Centre,
- Some fast-food chains
and even
- Bunnings!
There is also an AED locator App. you can download.
Don’t leave a casualty to get the defib always start CPR and send someone else to get the defib.
If you are by yourself and need an AED.. you have a problem. If there is one located within about 20 seconds from where you are, you can go and get it and put it on before you start CPR. Any further away than that and you need to start CPR without the Defib.

Can the defibrillator send a shock to someone who does not need it?
No, an AED only delivers a shock if it detects an abnormal heart rhythm. It will not shock a person with a normal heart rhythm or if their heart has stopped.
If the AED detects a normal rhythm or no rhythm at all, it will indicate that no shock is needed.
Can defibrillators be used on pregnant women?
Yes, a pregnant woman should be treated the same as any other person who is not responding or breathing. There are no contraindications to using an AED during pregnancy.
Can I use the defibrillator on a child?
Yes, from the age of 1yr old, we can apply a defib.
An AED will generally come with adult and child pads. Both sets of pads will have a diagram on them showing where to place them on the casualty. Child pads are smaller than adult pads for use with a child’s smaller chest.
If the available AED only has adult pads, you can still use them on a child up to eight years old. Just place one pad in the centre of the child’s chest and the other pad on their back between their shoulder blades.
After 8 years old we can treat a child the same as an adult and apply the pads according to the pad diagram. Make sure the pads do not touch or are close to each other.
Conclusion
- An Automatic External Defibrillator, also known as – Defib, AED, or Defibrillator – is an electronic device which assists with the resuscitation of an unconscious, not breathing casualty.
- The quicker you can apply an AED the more likely you can increase the chance of survival.
- AEDs can be located in public areas, shopping centres, sporting arenas and some businesses.
- They are simple to use.
Well, that’s that. Until next time….. Stay safe